In this article:
The skin is the largest organ of the body. It serves as the first line of defense against external irritants, germs, and other carriers of disease.

Open injuries, such as cuts, scrapes, burns, sores, insect bites, and surgical incisions, rupture the skin barrier and allow entry of bacteria or other germs, thus paving the way for infection.
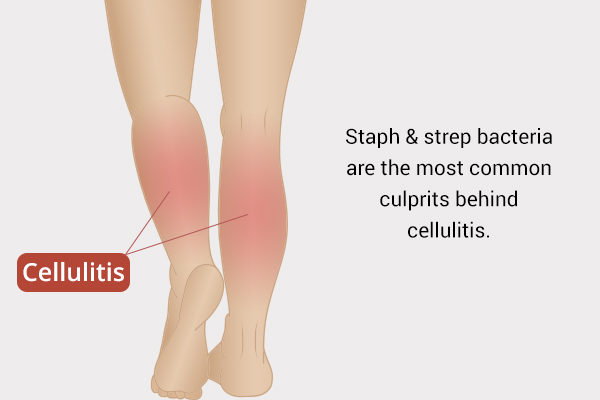
In the absence of proper wound care, bacteria can multiply at the site of injury and gradually spread to the deep layers of the skin. If the infection reaches the lower epidermis/dermis and subcutaneous tissue, it is referred to as cellulitis.
Cellulitis is an infection of the deep skin layers and subdermal tissue with symptoms of redness, swelling, warmth, pain, and in severe cases, blisters, pustules, and necrotic (dead) tissue.
How Common Is Cellulitis?
Cellulitis most commonly affects middle-aged men and older adults. In 2006, nearly 2,500 cases per 100,000 patients were diagnosed with cellulitis in the United States. (1)
A considerable mortality rate is attributed to cellulitis, which underlines just how dangerous it can be. A recent systematic review suggested that 0.7%–1.8% of all cases of cellulitis in the world result in death. (2)
Moreover, cellulitis is reported to be one of the top causes of visits to the emergency room. More than 200 people per 100,000 seek emergency help at the hospital for cellulitis every year. (3)
Where Does Cellulitis Occur?
Cellulitis can occur anywhere on the body, but it mostly affects the exposed areas of the skin, such as the face, neck, and limbs. Children most often get cellulitis on the head, face, or neck, whereas adults usually get it on the extremities.
Inserting an infected syringe into your skin can lead to the development of cellulitis, which is why it is very common in intravenous drug users.
Types of Cellulitis
Cellulitis is classified into different types depending on the site of infection. Some of the common ones are:
- Periorbital cellulitis: Bacteria infects the soft tissues of the eye socket located behind the orbital septum.
- Facial cellulitis: The infection affects the facial tissues, usually the cheeks, but can also spread to the adjoining areas behind or around the eyes, on the neck, or behind the ears.
- Breast cellulitis: Sweat and bacteria accumulate below the lower half of the breast, resulting in an infection.
- Perianal cellulitis: Infection or inflammation occurs in the area around the anal orifice.
- Preseptal cellulitis: The infection affects the eyelid skin but does not extend beyond the orbital septum into the orbit.
Causes of Cellulitis
The skin is naturally populated by multiple strains of bacteria that do not cause any harm so long as they are outside the body. However, any puncture or break in the skin barrier allows these pathogens to infiltrate the body and cause severe infection.
Staphylococcus and Streptococcus are the prime culprits behind cellulitis, with the majority of the cases attributed to group A beta-hemolytic Streptococcus, Streptococcus pneumoniae, and Staphylococcus aureus.
The following injuries or conditions can compromise the structural integrity of the skin and invite cellulitis:
- Skin trauma in the form of an insect bite, burn, sore, abrasion, or cut
- Insertion of a foreign object into the skin, such as a metal, glass, or infected syringe
- A puncture in the skin due to a surgical wound
- Dermatological problems, such as acne, eczema, psoriasis, or scabies
- An extension of some other infection, such as orbital cellulitis, which affects the eyelids and tissues surrounding the eye and can stem from a preexisting case of sinusitis
However, it can often be difficult or even impossible to identify the root cause of the infection.
Signs and Symptoms of Cellulitis
Cellulitis is often accompanied by the following symptoms:
- A painful rash with red, tender skin that may blister and scab over time
- Fever and chills
- Swelling in the glands or lymph nodes
- Bulging eyes due to the underlying inflammation
- Blurry or double vision
- Feeling exhausted despite no physical or mental exertion
- A general feeling of malaise or being unwell
- Nausea and vomiting
- Tight, glossy, stretched appearance of the infected skin
- Warm skin in the area of redness
- Bruising in the affected area
- Blisters at the infection site
Treatment for Cellulitis
Your doctor will prescribe antibiotics to control the growth and spread of the infection. The choice of drug will depend upon the type of bacteria responsible for the infection.
1. Antibiotics
The majority of cellulitis cases are caused by staph or strep bacteria and can be treated with the proper dosage of oral antibiotics, including beta-lactam antibiotics that fight against penicillinase-producing S. aureus.
The doctor usually prescribes a penicillin derivative or doxycycline/clindamycin/trimethoprim-sulfamethoxazole for individuals allergic to penicillin or those thought to have a methicillin-resistant Staphylococcus aureus (MRSA) infection. For more serious infections, IV antibiotics may be required. (4)
2. Topical medication
The most preferred topical options for treating cellulitis include anti-itch creams, antiseptic creams, and OTC antibiotic ointments such as Neosporin or Polysporin. These products not only hydrate and sanitize the affected skin but also speed up wound healing and mitigate the skin discomfort.
However, since your skin is already damaged and irritated, apply the cream gently instead of rubbing it, which will only aggravate the condition.
How Is Cellulitis Diagnosed?

Identifying the root cause of cellulitis involves reviewing the patient’s medical history and symptoms. This is followed by a physical exam to check for:
- Redness, warmth, tenderness, and swelling of the affected skin
- Signs of pus buildup or drainage at the site of infection
- Swollen lymph nodes near the affected area
The doctor may outline the area of skin redness with a pen to see if it extends beyond the initial site of infection over the next couple of days. This way, the doctor can track the spread of infection and see if it is responding to treatment or not.
Additional tests
If the injury involves the penetration of a foreign object into your skin or bone underneath it, the doctor may order an X-ray to see the depth of damage. The doctor may also conduct the following laboratory tests to identify the infection-causing bacteria:
- Skin swab test
- Blood culture
- Complete blood count (CBC)
- Culture of any fluid or material inside the affected area
- Biopsy to rule out other conditions that may be causing the symptoms
Risk Factors for Cellulitis
The following people are more susceptible to developing cellulitis and its complications:

- People who are middle-aged or elderly, especially men
- People with poor blood circulation
- People who have recently undergone surgery
- People who habitually take recreational drugs intravenously
- People with an impaired immune system due to certain medical conditions (cancer, AIDS, diabetes, malnutrition, and various other genetic illnesses) or immunosuppressive medications (corticosteroids)
- People who suffer from chronic illnesses such as diabetes
- People with preexisting skin conditions or disorders such as eczema, impetigo, and ringworm (tinea)
- People who are overweight or obese
- People with lymphedema as they have a damaged or overloaded lymphatic system that fails to filter toxins and waste from the blood and also hinders the circulation of lymph throughout the body
- People who have suffered from cellulitis in the past, especially of the lower leg, as they have a greater chance of getting it again (recurrent episodes)
- People who have undergone radiation treatment of the limbs
Those who are susceptible to cellulitis must exercise extra precautions when handling a skin wound.
Complications Associated With Cellulitis
Cellulitis infection can spread deep into the skin if not treated timely and properly. Worst-case scenario, the bacterial infection can enter the bloodstream and cause sepsis, which may lead to death.
Other complications associated with a mismanaged cellulitis include:
- Lymphedema
- Soft tissue abscess
- Infectious myositis
- Necrotizing fasciitis
- Osteomyelitis
- Thrombophlebitis (particularly in the elderly)
When to Worry About Cellulitis?
Cellulitis warrants urgent medical help if:
- The infection occurs on your face.
- If the wound or puncture covers a large area or is very deep.
- You get the infection after getting bitten by an animal or human.
- The redness is spreading very quickly from the original site of injury, despite the prescribed antibiotic treatment.
- The affected area becomes very painful, red, and warm to the touch – with or without fever and chills.
- You are running a high temperature or feeling very sick.
- You have chronic preconditions such as diabetes.
- You are immunocompromised, which means you have a condition such as cancer or HIV that has weakened or overburdened your body’s inherent disease-fighting ability.
- You have been receiving antibiotics intravenously, and the injection site is showing signs of inflammation or infection.
Call your doctor immediately if you notice any of these warning signs of a serious infection. Prompt medical treatment will help you avoid any serious risks or complications later.
Expert Answers (Q&A)
Answered by Dr. Anne Truitt, MD (Dermatologist)
Most cases of cellulitis are uncomplicated, and they usually resolve with oral antibiotics. Accurate diagnosis and prompt treatment are key. Cellulitis can be fatal if not treated appropriately and can spread to deep tissues and eventually to the lymph system, bloodstream, and organs.
Necrotizing fasciitis is a serious skin and soft tissue infection extending to the fascia. It is a medical emergency requiring IV antibiotics and surgical intervention. (4)
Uncomplicated cases of cellulitis do not usually lead to nerve damage. Untreated infections that spread to deep tissues or necrotizing fasciitis can cause permanent nerve damage due to the severity of the infection and increased likelihood of the need for surgical debridement (removal of dead tissue).
No, antibiotics are the mainstay of cellulitis treatment along with proper wound care, rest, limb elevation, NSAIDs, and other pain-relief therapies such as a warm or cool compress to promote quick healing.
No. Cellulitis does not spread from person to person.
There is a discrepancy in the recommendations of a warm or cool compress. Warm compresses are thought to dilate blood vessels, allowing more inflammatory/healing cells to the site and assisting with the release of any small abscesses.
Cool compresses are thought to be more relieving as the infection site is often warm. If you are keeping the site clean and covered, taking antibiotics, and resting, your choice of warm versus cold should be what makes you feel better.
It is not recommended to pop the blisters of an infection. This can introduce another nidus of infection. Simply keep the site clean and covered. Chlorhexidine (Hibiclens) is an over-the-counter antiseptic and a good choice for cleaning wound sites.
Clean wound sites with antibacterial soap and continue daily wound care until healed. If you have diabetes, wear protective shoes and check your feet often for injuries. Diabetes can cause nerve damage, making injury detection more difficult.
Protect your skin by wearing gloves when gardening, pants when hiking, and padding for elbows/knees when skating. Seek medical attention if you experience signs of redness, swelling, drainage, or fever.
Final Word
Cellulitis can develop due to a skin injury or other conditions. Its treatment depends on its underlying cause and other relevant health factors.
It is important that you consult your doctor about the proper antibiotic treatment for cellulitis instead of self-medicating, and complete the prescribed course to make a full recovery.
If you discontinue your medication as soon as you start feeling a little better, the infection will come back in full swing.

- Was this article helpful?
- YES, THANKS!NOT REALLY


