In this article:
Like water changes into ice at low temperatures, the skin can also freeze on being exposed to frigid weather conditions. This freezing of the skin and the tissues beneath it results in frostbite.

Body parts that generally remain exposed to the cold weather are prone to frostbite. These parts include the nose, toes, cheeks, chin, and ears.
Frostbite usually occurs on exposure to extremely chilly weather. However, mild temperatures intensified by conditions such as rain, wind, dampness, dehydration, low energy, or weak body can also cause frostbite.
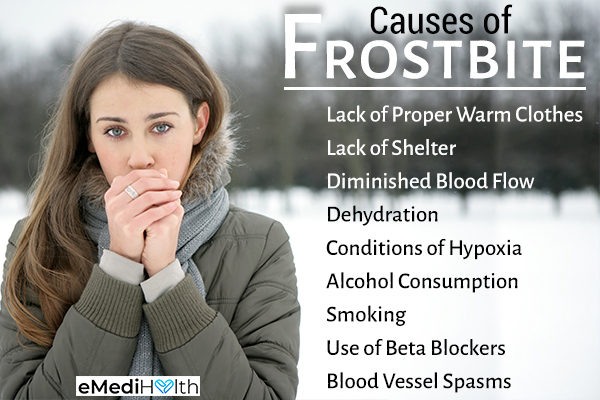
Causes of Frostbite
The body reacts to long-term exposure to cold weather by constricting the blood vessels of the extremities as they remain uncovered.
The narrowing of the blood vessels is the body’s way to conserve energy or body heat. It restricts blood supply to the extremities and redirects it to the vital organs instead, thus providing them adequate amounts of oxygen and nutrients. This also helps in keeping your body core warm.
If the blood supply to the extremities is not decreased, a greater amount of blood is exposed to the low temperature. This further reduces body temperature. A lack of blood supply causes the extremities to become cold and commences the hunting response, in which the dilation and constriction of blood vessels take place alternately.
The dilation is timed so that the temperature of the extremities can be maintained with a minimum amount of blood flow to those areas. This body mechanism helps retain the functionality of the extremities.
However, when there is a risk of hypothermia (body temperature around 96°F), the constriction sustains for long to prevent the exposure of vital organs to cold blood. Due to the restricted blood flow to the extremities, frostbite occurs.
The risk of frostbite increases at temperatures below 5°F (-15°C), (1) and chilly wind at a temperature of -16.6°F (-27°C) can speed up the process. Infants and older adults are more susceptible to frostbite than young individuals.
Different Stages of Frostbite
Frostbite occurs in three stages:
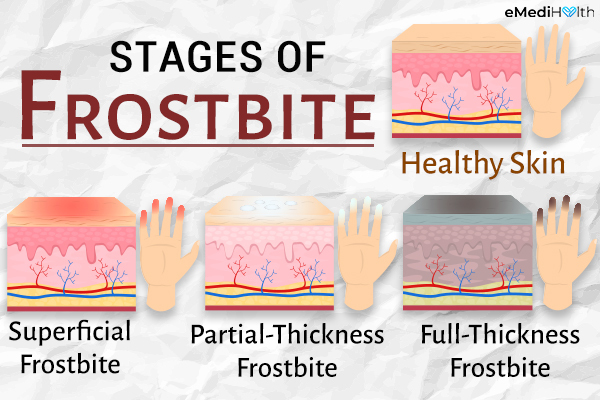
1. Superficial frostbite
Mild frostbite, also known as frostnip, is characterized by a change in the appearance of the skin. The affected areas may appear grayish or white and have a waxy touch.
It is generally a non-freezing injury. Warm water can be applied to the affected area, after which the skin may turn red and start peeling like in sunburn.
2. Partial-thickness frostbite
The affected parts of the body lose sensation. They become hard and may fail to regain original form after being pressed.
3. Full-thickness frostbite
The most severe degree of frostbite causes permanent tissue damage. If not treated on time, the affected tissue may become non-functional due to cell death and may turn black.
How to Know if It Is Frostbite?
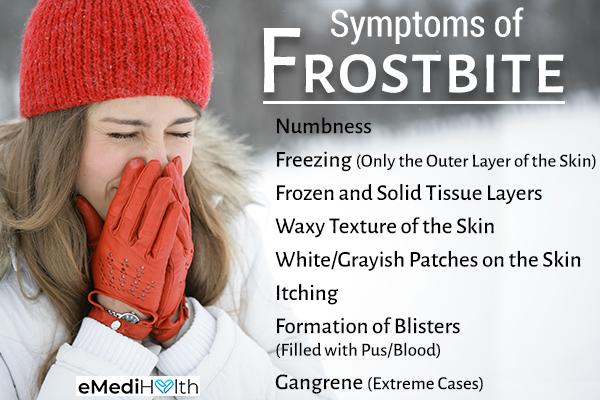
The symptoms of frostbite vary with each stage but commonly include the following:
- Numbness
- Freezing of only the outer layer of the skin while the tissue beneath it remains soft (superficial frostbite)
- Frozen and solid tissue layers (deep frostbite)
- Waxy texture of the skin
- White or grayish patches on the skin
- Itching
- Formation of blisters filled with pus or blood
- Gangrene (dead, black tissue) in extreme cases
Clinical Treatment for Frostbite
A mild case of frostbite or frostnip does not require medical attention and can be treated using at-home first aid. However, other cases of frostbite should be assessed and treated clinically.
It is necessary to provide first aid and check for hypothermia. On diagnosis, appropriate treatment is assigned, which can include medicines, rewarming therapy, surgery, and wound care.

The clinical treatment for frostbite depends on its severity:
- Oral antibiotics are prescribed if you develop an infection where blisters have formed.
- Removal of dead tissue by amputation or surgery is necessary to prevent the spread of infection.
- While rewarming, pain medications can be prescribed to help reduce the pain.
- Anti-inflammatory drugs are given to prevent swelling in the affected area.
- Intravenous injection (IV) may be administered to remove clots and help restore blood circulation.
- Hyperbaric oxygen therapy (HBO2) increases the oxygen-carrying capacity of the blood. This ensures that sufficient oxygen reaches areas of frostbite injury to alleviate ischemia. It also helps in preventing oxidative damage by increasing the supply of antioxidants to the affected areas.
- Administering a blood thinner or aspirin may help by increasing blood circulation. These medications can be taken after rewarming therapy within 24 hours.
It is important to avoid rubbing the affected area and prevent exposure to snow. Do not dip numb hands or feet in hot water as you might be unable to sense if the water is too hot.
Diagnosing Frostbite
Frostbite can be diagnosed by checking for the presence of visual symptoms such as skin discoloration and numbness. However, the severity of frostbite is difficult to estimate at once and requires a few weeks of treatment.
Laboratory tests such as MRI and X-rays can be performed to identify any complications occurring due to frostbite, which may be causing restricted blood flow or tissue ischemia.
You may not feel your tissues getting frozen as the cold can cause numbness. Thus, it is essential to recognize the early signs of frostbite, such as the tingling sensation associated with frostnip. Recognizing frostnip early enables you to take proactive measures for avoiding the complications of frostbite.
Risk Factors for Frostbite
The following factors may increase your risk of developing frostbite:
- Lack of proper warm clothes
- Lack of shelter
- Dehydration
- Conditions of hypoxia
- Alcohol consumption
- Smoking
- Use of beta-blockers (medications for cardiac problems) that lower the blood pressure
- Medical problems such as diabetes and hypothyroidism
- Diminished blood flow to the legs due to peripheral artery disease (PAD), wherein the blood vessels in the legs become hard and narrow
- Blood vessel spasms caused by the Raynaud phenomenon, which affect blood flow to the toes, nose, ears, and fingers and may occur due to emotional uproars or the cold weather (2)
Complications of Frostbite
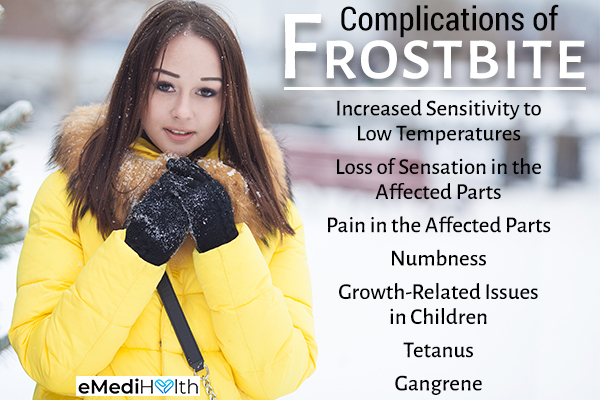
A severe case of frostbite may cause complications that may persist for a long time. These problems include:
- Increased sensitivity to low temperatures
- Loss of sensation in the affected parts, such as the fingers
- Pain in the affected parts
- Numbness
- Growth-related issues in children (if the growth plate of a bone is frostbitten)
- Tetanus
- Gangrene
When to See a Doctor
It is recommended to seek medical help in all cases of frostbite. You should seek immediate medical attention in the following conditions:
- Black or white discoloration of the skin
- Numbness in the affected area
- Symptoms of hypothermia
- Hard skin
- Persistent shivering or pain after rewarming
- Frostbite associated with injury
- Mumbled speech
- Inability to stand straight
- No effect of rewarming on the numbness or discoloration of the skin
- Development of blisters in the affected area
- Low body temperature (below 94°F)
Final Word
Frostbite causes damage to the tissues due to freezing, and deep frostbites can be life-threatening. An increase in the incidence of frostbite is found among the younger population who are taking risks in the name of recreational activities. It is vital to seek medical care immediately.
Timely treatment helps in preventing permanent tissue damage and regaining complete sensation in affected areas.

- Was this article helpful?
- YES, THANKS!NOT REALLY


