In this article:
Cirrhosis of the liver is a condition where the liver is scarred and permanently damaged. The liver is a very important organ of the body. It helps process nutrients, detoxify harmful substances, and produce important proteins.

When cirrhosis occurs, scar tissue replaces the healthy liver tissue, making it hard for the liver to do its job properly. (1)
The tricky part is cirrhosis doesn’t always show itself right away. In fact, many people don’t even realize they have it until their liver is severely damaged.
It can take years for the symptoms to show up, and they can be vague, such as loss of appetite, feeling tired all the time, and losing weight. As the disease progresses, you may experience problems such as high blood pressure in the liver, fluid buildup in the abdomen (ascites), and, in severe cases, liver failure.
To diagnose cirrhosis, doctors often need to take a small piece of your liver for examination. (1)(2)
Unfortunately, cirrhosis is usually a permanent and irreversible condition. The treatment mainly focuses on providing support to manage the symptoms and complications associated with the disease.
That’s why it’s important to take care of your liver and get regular checkups.
Causes Responsible for Cirrhosis of the Liver
Cirrhosis can stem from the following causes: (2)
- Excessive alcohol consumption can damage the liver and lead to cirrhosis.
- Nonalcoholic fatty liver disease can also contribute to cirrhosis. This condition involves having too much fat stored in the liver, and it can cause problems if not managed properly.
- Chronic hepatitis B, C, and D contribute to cirrhosis.
- Sometimes, your own immune system goes haywire and attacks your liver. This condition is called autoimmune hepatitis and can be a sneaky cause of cirrhosis.
- Diseases that affect the bile ducts such as primary sclerosing cholangitis (bile duct inflammation) can also lead to cirrhosis.
- Sometimes, certain liver diseases run in families due to genetic factors.
- Long-term use of certain medications can also cause liver problems. So, make sure to follow your doctor’s advice and be mindful of the medications you take. Isoniazid, methotrexate, and methyldopa, if taken as self-medication without monitoring, can damage the liver.
- Chronic heart failure can sometimes lead to liver congestion, where blood flow out of the liver slows down.
- Congenital disorders, such as hemochromatosis (iron overload), Wilson’s disease (copper buildup), and galactosemia (difficulty processing galactose) can lead to cirrhosis.
- Poor nutrition, especially a diet low in proteins such as methionine and choline, can lead to fatty liver and cirrhosis.
- Infections such as malaria and kala-azar can indirectly contribute to cirrhosis by causing malnutrition.
Risk Factors of Cirrhosis
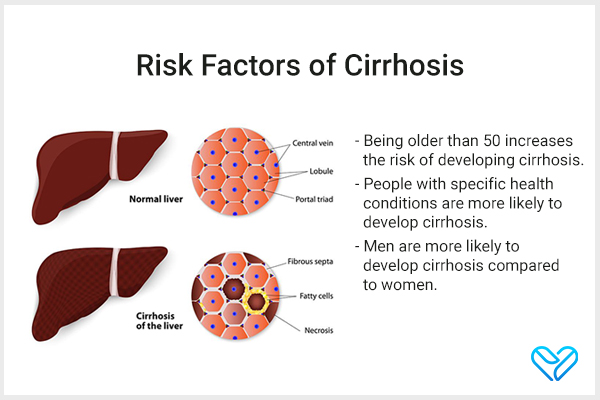
Cirrhosis is not uncommon. Researchers estimate that around 1 in 400 adults in the United States have cirrhosis. So, you’re not alone if you’re dealing with this condition.
The risk factors of cirrhosis are as follows:
- Being older than 50 increases the risk of developing cirrhosis. Cirrhosis tends to be more common in adults between the ages of 45 and 54 years. In fact, about 1 in 200 adults in this age group in the United States has cirrhosis. (1) Note: However, it’s important to note that cirrhosis can affect people of any age.
- People with specific health conditions are more likely to develop cirrhosis. These include individuals who have abused alcohol for a long time and those with type 2 diabetes.
- Men are more likely to develop cirrhosis than women. The reasons behind this are still being studied, but it’s an important factor to be aware of. (1)
Symptoms of Cirrhosis
In the early stages, cirrhosis may not show any signs or symptoms. So, it’s possible to have it without you even realizing it. However, later on, several symptoms will show: (2)
- As cirrhosis progresses, you may start feeling tired and weak, lacking energy to do your daily activities.
- You might experience a decrease in appetite, not feeling as hungry as usual.
- Without trying, you may notice that you’re losing weight.
- You might experience feelings of nausea and occasionally vomit.
- You may feel mild pain or discomfort in the upper-right side of your abdomen, where your liver is located.
- You may experience confusion, difficulties with thinking, or memory loss as cirrhosis can affect your brain function.
- You may have swelling in the lower legs, ankles, or feet, which is a common symptom of this condition.
- Fluid buildup can occur in your abdomen, leading to bloating.
- You experience severe itching, making your skin feel irritated and uncomfortable.
- You may notice that your urine becomes darker in color. Additionally, you might develop jaundice.
Note: It’s crucial to know that cirrhosis can go unnoticed for a long time. In fact, about one-third of people with cirrhosis never experience any symptoms.
Treatment for Liver Cirrhosis
There is no specific cure for cirrhosis, but the underlying causes can be managed and further damage can be prevented. On average, the survival rate for people with cirrhosis can range from 10–12 years.
The outlook for cirrhosis depends on different factors such as the cause, severity, complications, overall health, and effectiveness of treatment. (3)
Treatment for cirrhosis involves:
- Medications are often prescribed to treat the diseases that caused cirrhosis in the first place. These medications can slow down the progression of cirrhosis and prevent liver failure.
- Along with medications, it’s important to make supportive changes such as stopping the use of harmful drugs, providing proper nutrition with extra vitamins, and treating any other related disorders and complications.
- Medications include ursodeoxycholic acid and cholestyramine for itching.
- For those with varices (enlarged veins in the esophagus or stomach), therapy is needed to prevent bleeding.
- In severe cases of liver failure, a liver transplant may be necessary.
Note: It’s important to note that continuing to drink alcohol, even in small amounts, greatly worsens the prognosis.
Testing for and Diagnosing Cirrhosis
To figure out what’s causing cirrhosis, doctors will gather important information about your health history and do a thorough examination. The main diagnostic tests are blood tests, imaging tests, and biopsy.
Blood tests
Your doctor will recommend blood tests to check for abnormalities in liver enzyme levels, which can indicate liver damage. Laboratory tests alone may improve suspicion of cirrhosis but cannot confirm it.
Liver functioning tests (LFT) are done to look for increased levels of liver enzymes such as ALT, AST, and ALP, as well as increased bilirubin levels and decreased blood protein levels.
They may also test for viral infections such as hepatitis B or hepatitis C and for autoimmune liver conditions using specific antibody tests. (4) Serologic tests are used to detect viral load.
Imaging tests
Imaging tests help doctors visualize the liver and assess its condition. These tests can show the size, shape, texture, and stiffness of the liver. Stiffness measures can indicate the presence of scarring and help determine its severity.
Imaging tests include magnetic resonance imaging (MRI), ultrasound, X-rays such as computerized tomography (CT) scans, and a special ultrasound called transient elastography. (4)
Experts share how in advanced cirrhosis, ultrasonography shows a small, nodular liver and also detects portal hypertension or ascites.
Biopsy
In some cases, a liver biopsy may be performed. This procedure involves taking a small sample of liver tissue to examine it closely.
A liver biopsy can provide a definitive diagnosis of cirrhosis and determine the extent of scarring. It can also help identify the underlying cause of cirrhosis or detect liver cancer. (4)
Complications of Cirrhosis
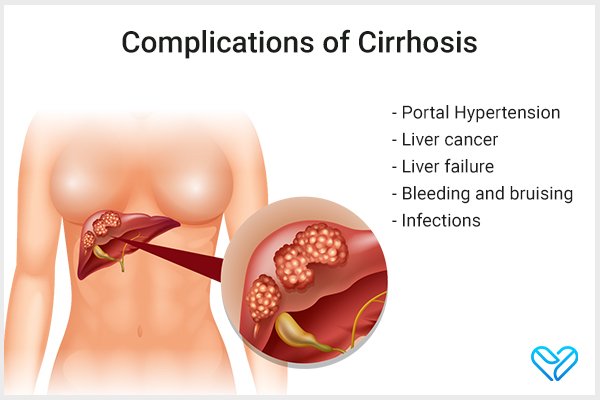
Complications can arise as the disease progresses, and sometimes, these complications are the first signs that something’s wrong.
1. Portal hypertension
Portal hypertension is the most common serious complication of cirrhosis. It happens when scar tissue partially blocks the normal blood flow through the liver, leading to high blood pressure in the portal vein.
It can also lead to swelling in the legs, ankles, or feet (edema) and fluid buildup in the abdomen (ascites), which can result in a serious infection. (1)(5) It can further cause gastrointestinal bleeding from varices (enlarged blood vessels) in the esophagus, stomach, or rectum.
2. Liver cancer
Having cirrhosis increases the chances of developing liver cancer. In fact, most people who develop liver cancer already have cirrhosis. (1)(6)
3. Liver failure
In some cases, cirrhosis can progress to liver failure, where the liver is severely damaged and stops functioning properly. This may require a liver transplant. (1)
4. Bleeding and bruising
As liver function worsens, you might notice that you bruise more easily and bleed more than usual, even from minor cuts or injuries. (2)
5. Infections
Cirrhosis weakens the immune system, making you more prone to urinary tract infections, tuberculosis, abdominal bacterial infections, and pneumonia. (1)
6. Other complications
- Fluid buildup: Cirrhosis may cause fluid buildup in the abdomen, leading to possible hernias.
- Weaker bones: Cirrhosis can result in weak bones and a higher risk of fractures (osteoporosis).
- Gallstone formation: Bile flow disruption due to cirrhosis can cause gallstone formation.
- Medication sensitivity: People with cirrhosis may be more sensitive to medications due to liver processing difficulties.
- Increased risk of type 2 diabetes: Cirrhosis raises the likelihood of developing type 2 diabetes.
Note: These complications can be life-threatening and can significantly impact a person’s health and overall well-being. If not properly managed, cirrhosis can progress to a point where the liver can no longer perform its vital functions, leading to organ failure and potentially death.
The Child-Pugh Scoring System
The Child-Pugh scoring system is used by doctors to assess disease severity and predict outcomes in patients. It is a way to predict the risk of mortality in people with cirrhosis.
This scoring system was created in 1964 by Child and Turcotte to help determine which patients would benefit from certain surgeries. They divided patients into three groups based on the severity of their liver function: A, B, and C.
The scoring system looks at five factors: bilirubin levels in the blood, albumin levels in the blood, the presence of ascites (fluid buildup in the abdomen), neurological symptoms, and the overall nutritional status of the patient. (7)
Final Word
In conclusion, cirrhosis of the liver is a condition where scar tissue replaces healthy liver tissue, making it difficult for the liver to function properly. It can be caused by various diseases.
While there is no cure, treating the underlying causes and making lifestyle changes can slow its progression. Regular checkups, avoiding alcohol and certain medications, and taking care of your overall health are essential in managing cirrhosis.
Remember, early intervention is key, so seek medical advice if you suspect you may have cirrhosis.
 Continue Reading9 Home Remedies for Cirrhosis of the Liver and Preventive Tips
Continue Reading9 Home Remedies for Cirrhosis of the Liver and Preventive Tips
- Was this article helpful?
- YES, THANKS!NOT REALLY


