In this article:
Vaginal delivery refers to the natural process of giving birth through the vagina. It is typically performed without the use of any medical intervention, barring the assistance of the medical staff.

The OBGYN will guide the entire process in light of the relevant screening tests and the patient’s overall health condition to steer clear of any complications during or after delivery.
The doctor can switch to an assisted delivery or even a cesarean anytime during the labor process to circumvent any unforeseen problem. The doctor will choose the best delivery method to ensure the wellbeing of both the mother and baby.
What Is a Normal Delivery?
Patients ask me all the time about having a normal delivery. As a high-risk pregnancy physician, I define normal delivery as one in which there were no complications during the pregnancy, regardless of how the baby is delivered. Therefore, while most patients consider only vaginal deliveries to be normal, you can also have a normal Cesarean delivery.
Cesarean section is completely normal, considering 31.9% of women in the United States deliver their babies this way, as reported by the Centers for Disease Control and Prevention. (1) Thus, a third of deliveries cannot be considered abnormal.
We should be careful in describing normal deliveries only as vaginal deliveries as this could shame mothers that have to undergo Cesarean sections to deliver their babies.
Process of a Normal Vaginal Delivery
A normal vaginal delivery occurs when a full-term pregnant woman delivers her baby vaginally and does not require instrumentation or devices, such as vacuums or forceps, to push the baby out. So, not all vaginal deliveries are considered to be normal.
A woman may need an operative vaginal delivery, such as a forceps-assisted or vacuum-assisted vaginal delivery, in case a complication occurs during labor.
First Sign of Labor

Most low-risk women will experience contractions as the first symptom of labor. Other symptoms include vaginal spotting or a bloody mucus discharge and rupture of membranes (referred by many patients as breakage of their water).
Once you experience one of these symptoms, contact your provider for further instructions or go to the hospital to be assessed. Your provider will need to check your cervix to see if you have started to dilate.
Different stages of active labor
Once you reach 6 cm of cervical dilation with regular contractions, you are considered in “active labor.” During active labor, you may experience uterine contractions about every 2–3 minutes.
Stage 1
The first stage of active labor refers to the time it takes the cervix to dilate from 6 cm to 10 cm. However, the dilation required for a successful vaginal delivery may vary from patient to patient.
Many factors play into the time it takes to fully dilate, such as:
- Number of previous deliveries
- Maternal weight
- Type of maternal pelvis
During this process, the patient should expect to experience some vaginal bleeding and rupture of membranes. For some women, the provider will artificially rupture the membranes as a way to continue to stimulate the labor process.
Stage 2
Once 10 cm of cervical dilation is reached, the patient will be instructed to push. This begins the second stage of labor, which lasts for anywhere between 20 minutes and a few hours.
During this stage, patients can continue to have vaginal bleeding and painful contractions. Moreover, the patient experiences pressure and the natural urge to push, because of which, women actually have bowel movements during labor. This is normal and nothing to be embarrassed about.
Stage 3
Once the baby is delivered, the third stage of labor starts, which involves the delivery of the placenta, also known as the afterbirth. This stage can take up to 30 minutes. It is normal to experience mild contraction, cramping, and vaginal bleeding after placental delivery.
Correct Technique to Push During Labor
Pushing during labor is a tough but very important job, which has to be done correctly to avoid early exhaustion or other complications.
I encourage patients to push only during contractions, which should occur about every 1–2 minutes and last around 30–90 seconds once the cervix is fully dilated.
When instructed to push, patients should bear down like they are having a bowel movement and hold this effort for at least 10 seconds before relaxing. If the contraction is still present, the patient will be instructed to push again. In between contractions, the patient will be encouraged to relax.
Pushing without the help of a contraction can increase exhaustion and cause vaginal swelling.
Challenges in Normal Vaginal Delivery
Inadequate pushing, especially for first-time moms, is a challenge in a normal vaginal delivery. Pushing is hard work and many patients over exhaust themselves.
Patients should remember to push only during contractions. Many women scream while pushing due to pain or frustration, which can redirect energy away from pushing. This brings me to the second challenge, which is pain control. Many women want to deliver without pain medications or an epidural.
So, during the labor process, patients can experience intense and frequent painful contractions and a burning sensation as the baby crowns. This pain can distract them from pushing when they should get ready to push as the pain intensifies instead.
How Long Does It Take to Deliver a Baby?

The total labor process can vary based on several factors, such as:
- Number of previous deliveries
- Maternal habitus
- Pelvis type
- Whether a patient chooses to have an epidural
According to the Friedman labor curve, the entire labor process can take up to 30 hours, which is divided as follows:
- Latent labor, or the time before the cervix reaches 4 cm of dilation, can take up to 20 hours during the first pregnancy and 14 hours for those who have previously had a vaginal delivery.
- Active labor can last for 7 hours for first-time moms and around 5 hours for women who have given vaginal birth before.
- The pushing could take up to 3 hours for first-time deliveries (4 hours with an epidural) or 2 hours with previous vaginal deliveries (3 hours with an epidural).
Can Childbirth Be Stressful for the Mother and Baby?
During the normal labor and delivery process, stress-associated hormone increases in both the patient and baby. This increase in hormone is a good thing in that it helps prepare the baby for life outside of the uterus and the mom for breastfeeding.
Lower levels of stress-related hormones have been seen in patients delivering vaginally and higher in patients with operative vaginal deliveries. The significance of long-term neonatal outcomes is unknown. (2)
Comparative Pain of Vaginal Delivery and C-section
During the process, yes, but long term, no. A vaginal delivery can mean experiencing painful uterine contractions for over 24 hours.
The contractions stop almost immediately following delivery and most women experience cramps similar to menstrual cramping for a few days. These are usually manageable with NSAIDs, such as Motrin. Therefore, recovery after delivery is quick.
In contrast, while no pain is felt during a Cesarean section, the recovery tends to be much longer.
Simple Tips to Normal Vaginal Delivery
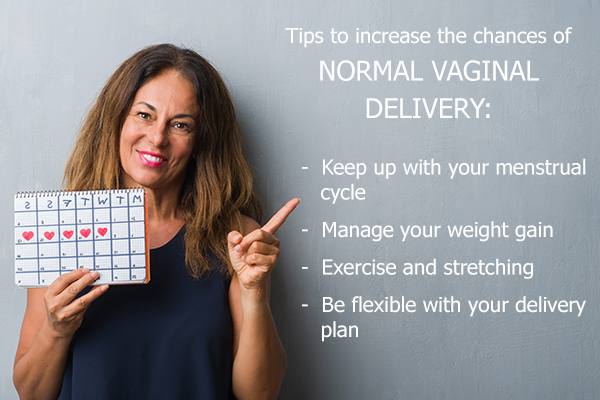
There is no definite way to ensure that a patient has a vaginal delivery. However, the following are ways to increase the chances of a normal vaginal delivery:
1. Keep up with your menstrual cycle
This is important to ensure correct pregnancy dating. If dates are not accurate, that could lead your provider to believe you are too far along or think that your baby is too small, both requiring induction of labor.
Inductions increase the rate of Cesarean section compared to patients presenting with symptoms of active labor.
2. Manage your weight gain
Patients should gain about 15–30 lbs during pregnancy (for obese patients, they should gain 11–20 lbs). Patients who are morbidly obese have a higher rate of Cesarean section. So, managing weight gain by eating a well-balanced diet is beneficial.
3. Exercise and stretch
Exercise not only helps with weight gain but also helps with a lower rate of gestational diabetes and blood pressure issues in pregnancy. (3) Both of these complications are associated with a higher rate of induction of labor, preterm delivery, and need for Cesarean section. (4)(5)
All said and done, you must still be flexible with your delivery plan. Having a plan is great. However, it can be dangerous to decline interventions that are needed to keep you and your baby safe.
Complications Associated With Vaginal Childbirth
Complications that can arise during the labor and delivery process include vaginal bleeding, fetal distress, or maternal complications.
The following measures are taken to prevent these complications:
- Patients are monitored constantly during the labor process for signs of these complications.
- Pads are evaluated by nurses every 1–2 hours to ensure that bleeding is not too heavy.
- The baby’s heart rate is monitored frequently or continuously to make sure there are no decelerations in the baby’s heart rate.
- The patient’s blood pressure, temperature, lungs, and extremities are checked frequently to make sure there are no issues with high blood pressure, signs of infection, respiratory distress, or abnormal reflexes.
- Abnormalities found could mean that a patient needs further attention and/or operative delivery to safely get both the patient and baby through the delivery process.
Final Word
I encourage patients to speak with their providers about their delivery concerns and what to expect before confirming the delivery plan. Some interventions are necessary to keep you and your baby safe.
Refusing certain interventions can lead to an emergency Cesarean section or fetal or maternal complications that can be long-lasting.
- Was this article helpful?
- YES, THANKS!NOT REALLY


