In this article:
Temporomandibular joint and muscle disorders, commonly called TMD, refer to a heterogeneous group of musculoskeletal and neuromuscular conditions that affect the temporomandibular joint (TMJ).

These conditions lead to the misalignment of the complex system of muscles, ligaments, discs, and bones that form the TMJ, preventing them from working as well as they should.
Temporomandibular joint dysfunction (TMD), also known as TMJ syndrome, is often characterized by pain and tightness in and around the TMJ, which can make basic functions such as speaking and eating increasingly difficult. (1)
What Is TMJ?
The temporomandibular joint (TMJ) is one of the complex structures in the body that are made up of muscles, tendons, blood vessels, nerves, and bones.
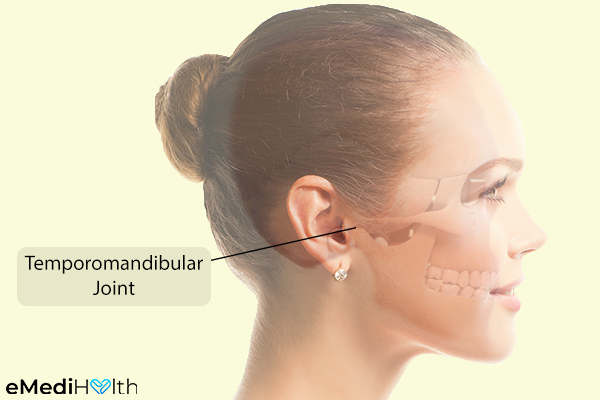
On both sides of your head in front of your ears, you have a pair of temporomandibular sliding joints that connect the lower jawbone to your temporal bone on the side of the skull.
The facial muscles that make it possible for you to open and close your mouth are attached to the TMJ. In fact, the movement of the jawbone itself is controlled by the TMJ, which can rotate and move forward, backward, and side to side.
Types of TMD
Researchers generally agree that TMD conditions fall into three main categories:
1. Facial muscle imbalance
One common form of TMD is characterized by myofascial pain, which is caused by facial muscle imbalance due to incorrect chewing habits or unfavorable facial expression habits.
The pain and discomfort in the muscles that control jaw function will initially be more noticeable on the looser side and can gradually be felt in and around the affected joint.
2. Internal derangement of the TMJ
TMD can also stem from internal derangement of the TMJ, possibly due to disc displacement, jaw dislocation, or injury to the rounded ends of the lower jaw known as condyle.
You may also experience a locked jaw, the inability to open your mouth, especially immediately after waking up in the morning. The pain often develops on one side of the jaw initially. (1)
3. Arthritis
Arthritis affects TMJ, just as it affects other joints in the body. Osteoarthritis can cause progressive degeneration of your TMJ due to the loss of cartilage. Rheumatoid arthritis, on the other hand, is associated with the inflammation of the TMJ, which can also cause deformation of the joint in extreme cases.
What Causes TMD?

TMD is commonly caused by the following:
- Malocclusion or poor positioning of your upper and lower teeth such that they do not fit together properly is the primary cause of temporomandibular disorders. (2)
- In many cases, TMD is triggered by some trauma or injury to the jaw bone, joint, or adjoining muscles.
- People with preexisting arthritis are at a higher risk of developing TMD due to the gradual degeneration of the joint brought about by this disease.
- People born with certain structural defects in the jaw are more likely to develop this disorder.
- Getting dental work done can also trigger pain in the TMJ, as the joint is stretched open for extended periods of time.
- People who are in the habit of clenching or grinding their teeth or chewing gum, a pen or pencil, or their fingernails are more likely to develop this condition.
- Wearing ill-fitting partial or full dentures can also pave the way for TMD.
- The use of orthodontic braces can also make you more prone to this kind of problem.
- Poor body posture can exert undue strain on your neck and facial muscles, making you more prone to TMJ pain.
- Not getting enough sleep and nutrition can also contribute to the onset of TMJ syndrome.
- During pregnancy, women secrete a hormone that causes their joints to relax and soften, which may worsen TMJ pain.
What Are the Symptoms of TMD?
The signs and symptoms of TMD may show up on just one side of the face or both. Common signs and symptoms of TMD are:
- Dull, aching pain in the jaw joints and facial muscles, which may radiate to the cheeks, neck, shoulders, and back
- Pain that may persist at resting position and worsen while eating, talking, or simply opening the mouth
- Difficulty biting or chewing food
- Pain that may cause an earache, a ringing or buzzing sensation in the ear, numbness in the ear, and possible hearing loss
- Limited movement of the jaw
- Tenderness in and around the affected TMJ
- Unusual clicking, popping, or grating sound when opening or closing the mouth, which is accompanied by pain and limited movement of the jaw
- Difficulty opening or closing your mouth
- Tension headaches and/or migraines
- An affected joint that gets stuck or “locks” when opened widely and becomes difficult to close
- Pressure behind the eyes and blurred vision
- Sore, stiff, and tight neck muscles and jaw
- Muscle spasms in the jaw when the joint becomes overstretched
- Swelling of the face and mouth on the affected side
- Dizziness, vertigo, and nausea
Medical Treatment for TMD

In most cases of TMD, proper self-care and lifestyle changes are more than enough to resolve mild-to-moderate symptoms. Your doctor may recommend the following treatment options: (3)
- TMJ patients may be given biofeedback training to help them manage their involuntary stress responses such as stiffening of the jaw muscles, which may exert undue strain on the TMJ joint.
- If over-the-counter pain medications fail to provide considerable relief, your doctor could prescribe muscle relaxants, analgesics, tricyclic antidepressants, nerve pain medications, sedatives, anti-anxiety drugs, and anti-inflammatory medications but only for a short period of time.
- If the TMJ syndrome is caused by involuntary grinding and clenching of the teeth during sleep, you may be advised to wear a prosthodontic appliance such as a night guard (bite guard) or an oral splint (bite plate).
- People whose TMD stems from a preexisting degenerative condition such as osteoarthritis are often prescribed steroid injections for temporary or permanent relief from the discomforting symptoms associated with this condition.
- In some cases, Botox injections may be used to relax the jaw muscles that control chewing.
- Surgery is the last resort for TMD treatment and is only recommended when there is something wrong with the actual joint itself. Some cases can be resolved by minimally invasive procedures such as TMJ arthrocentesis or arthroscopy, whereas others warrant an open-joint surgery to fix the structural problems in the joint. In rare cases, when the movement of the jaw becomes extremely limited and the symptoms are long-lasting, a total joint replacement may be needed.
How Is TMD Diagnosed?
Diagnosing TMD usually involves the following steps:
- Your doctor will consider all your symptoms and proceed with a thorough examination of your dental cavity to see if your teeth are properly aligned.
- The area around the jaw and the head will be pressed to locate the sensitive or painful sites.
- The doctor will check the range of motion of your jaw and may ask you to slide your teeth from side to side. He/she will closely watch, feel, and listen to your jaw as you open and shut your mouth.
- The doctor may even order a few imaging tests, such as dental X-rays, CT scan, MRI, and TMJ arthroscopy, to detect any structural abnormalities with the teeth, surrounding tissue, and jaw or cranial bones.
Your doctor may then send you to an oral and maxillofacial specialist, an ENT specialist, or a dentist specializing in jaw disorders to confirm the diagnosis.
Risk Factors for TMD
The following medical conditions may increase your risk of TMD:
- Women between the ages of 18 and 44 years are more prone to developing TMJ syndrome than men. The risk is particularly high among women in their childbearing years, and so a possible link between the female hormone estrogen and TMDs is suspected.
- TMD is also more prevalent among people who grapple with preexisting ailments characterized by chronic pain, such as lower back pain and headaches.
- People who have a poor neck and back posture often suffer from neck strain and malfunctioning jaw muscles.
- Stress is often held responsible for increased muscle tension in the jaw, which leads to increased clenching and sets the ground for TMJ syndrome.
- Patients with chronic inflammatory arthritis, which includes osteoarthritis, rheumatoid arthritis, and fibromyalgia, are more likely to develop this disorder.
- People with jaw or facial deformities, jaw trauma including fractures and dislocations, misaligned teeth (crooked teeth), or a misaligned bite have an increased risk.
- Certain inherited factors such as a low threshold for pain and increased stress responses can also make one more likely to develop TMJ syndrome.
- Certain genetic factors related to psychological health and inflammation may increase the risk for TMJ syndrome as well.
When to See a Doctor

A visit to the dentist is called for if you experience the following symptoms that may indicate a possible case of TMD:
- Difficulty in jaw movements
- Intense pain in and around the jaw area
- Clicking and popping sounds when you move your jaw
If your jaw becomes locked in a wide-open or closed position, you are advised to get yourself to a hospital’s emergency department.
Expert Answers (Q&A)
Answered by Dr. Jeffrey L. Brown, DDS (Dentist)
The recovery time for TMD depends on:
• How long it takes for the discs to move back into proper position
• Whether the distortions to the cranial bones correct in a short period or for a long time
I generally tell our new patients that I need to work with them for about a year, and then we re-assess where we are at.
Not at all. In almost all cases, we are able to help TMD patients, and they are able to return to most normal activities. Think of it like a broken bone – you wear a cast for a while, then do physical therapy and rehab, and then go back to normal life.
If you wait too long and ignore the initial signs of TMD, damage may occur, which is more difficult to treat. In those cases, TMD treatment and then a possible surgical intervention will be needed to help reduce inflammation in the joints.
When the discs in the joints are out of place, they tend to rub against the condyle/jaw bone, and inflammation builds up.
Chronic inflammation can lead to erosion of the condyles and degenerative arthrosis, which is difficult to repair.
It can lead to a need for total joint replacement, but none of our patients have ever had to do that because we treat them long before it goes that far.
We advise all our patients with TMD to do a hot bath each night with Epsom salts and lavender or chamomile to reduce inflammation. Massaging the face and the joints will help to loosen muscles.
It is also important to not lift heavy objects or work out too hard at the gym as your body is trying to heal. If you have TMD, you do not want to stress out the joints. Stick to a soft food diet. Apply alternate heat and ice on the jaw joints.
Meditation and yoga are also great ways to reduce stress. Stress causes grinding and clenching in the jaw joints, which irritate the jaw joints when TMD is present.
Throughout the day, try and keep your tongue on the roof of your mouth, with your teeth apart and lips closed. Doing so will help take the pressure off the jaw joints as well. You can also do many at-home myofunctional exercises to relieve the pain.
Absolutely. When the discs are displaced in the jaw joints, inflammation in and around the ear canal may result, which can cause tinnitus.
Tinnitus is a very, very common TMD symptom that can also occur when the discs have been out of place for a long period.
Sometimes. As you lay back and the jawbones or condyles slip back into the sockets, more pressure may be placed on the discs and cause more pain.
Also, at night, people are more prone to grinding and clenching their teeth. When TMD is present, a person may wake up with a lot of facial and jaw pain.
I try to explain to our patients that a slipped/displaced disc is like having a broken bone. You need to “set” it so it can heal. Our office creates non-invasive customized dental appliances to help take the pressure off the jaw joints and align the cranial bones.
So when we put our appliances into place, we allow the joints to heal and give the discs a chance to get back into proper position. When pressure on the jaw joint area is reduced, the symptoms of TMD start to dissipate.
We have had great success in helping patients conservatively using ALF, modified splints, and sleep appliances. The clicking and popping sounds of the jaw are the early warning signs that you have a problem and should deal with it as soon as possible.
Early treatment gives us the best chance to fix things in the simplest way possible! TMD was barely taught in dental school, so many dentists are not aware of this problem or don’t take it seriously enough.
We hear all of the time, “if the popping and clicking in your jaw don’t hurt, don’t worry about it!” This is simply not true. Please take initial TMD symptoms seriously so you can easily fix the problem, instead of waiting until you are experiencing pain.
Final Word
Most patients with TMD do not require extensive medical care to improve their condition. The symptomatic discomfort associated with an uncomplicated case of TMJ syndrome usually resolves with simple self-care practices and prescribed home treatment.
That said, early treatment is the only way to ensure a fast recovery. If left untreated, even a simple case of TMD can evolve into something serious that may take much longer to heal.

- Was this article helpful?
- YES, THANKS!NOT REALLY



