In this article:
Polycystic ovary syndrome (PCOS) is an endocrine disorder that affects women of reproductive age, but its symptoms may persist well beyond menopause.
It is characterized by an excess of androgens, which are male sex hormones that are found in both genders. Thus, women with PCOS tend to have abnormally high levels of androgens, which hamper the functioning of their ovaries and thwart the ovulation process.
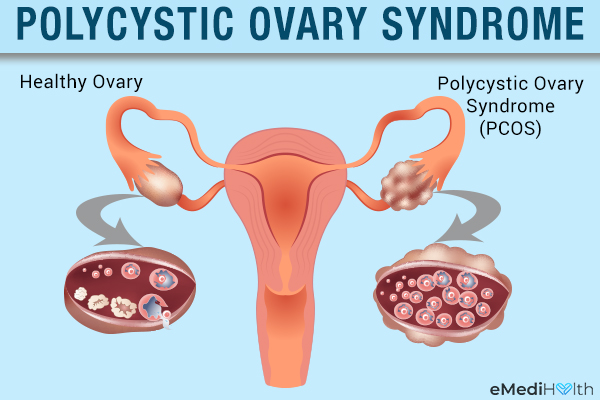
The ovary releases a mature egg into the fallopian tube every month, which if fertilized by a sperm leads to a pregnancy.
Given that ovulation is an essential prerequisite for pregnancy, PCOS can make it very difficult for a woman to conceive by causing anovulation, or lack of ovulation in a menstrual cycle.
In fact, PCOS is regarded as one of the leading causes of both anovulation and female infertility. A lot of women with PCOS become aware of their condition only after getting tested for infertility issues.
How Common Is PCOS?
PCOS is the most prevalent hormonal disorder among menstruating females, affecting 4%–8% of all women of childbearing age. (1) It is estimated that 1 in every 10 such women suffers from it.
In the United States alone, 6%–12% of females are diagnosed with PCOS during their childbearing years, which translates to approximately 5 million women. (2)
Causes of PCOS
While the exact cause of PCOS remains unidentified, it is typically related to a hormonal imbalance in the woman’s body.
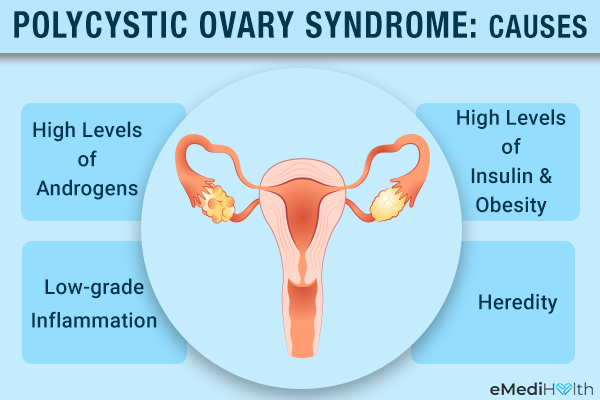
1. High levels of androgens
All women secrete a minimal quantity of male hormones, but in women with PCOS, the ovaries produce abnormally high levels of androgens. The ovarian function is negatively affected when there is an excess of these hormones in the female body.
This type of hormonal imbalance can prevent the ovaries from releasing a mature egg during each menstrual cycle. This can cause irregularities in the menstrual cycle and fertility issues.
2. High levels of insulin and obesity
Insulin is a peptide hormone that plays a critical role in the regulation of blood sugar levels and the conversion of food into energy.
Researchers have also observed a link between increased levels of insulin and the corresponding increase in the secretion of male hormones in some women. Thus, in effect, it can be said that high levels of insulin stimulate the ovaries to produce more male hormones. (3)
3. Low-grade inflammation
Another common characteristic found in many women with PCOS is they suffer from a type of low-grade inflammation that triggers their ovaries to secrete high levels of the male hormones.
Over time, this excess of androgens can pave the way for heart and blood vessel problems. (4)
4. Heredity
Genetics is also considered an important factor as PCOS tends to run in families. If your mother or sister has PCOS, you have a 50% chance of having it as well.
Symptoms of PCOS
Women with PCOS usually have at least two of the following three conditions: (5)
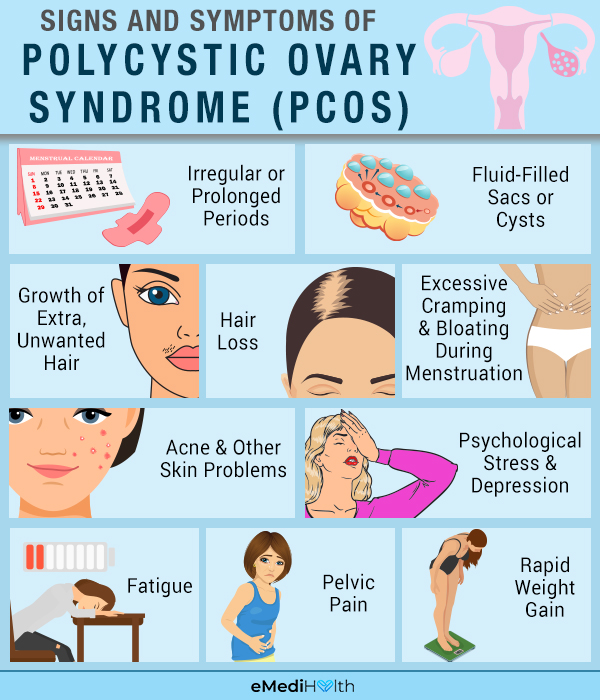
- The ovaries fail to release an egg regularly, leading to an unstable menstrual cycle. The absence of ovulation is characterized by irregular or prolonged periods (abnormal mensuration) and, in some cases, cessation of periods altogether (amenorrhea).
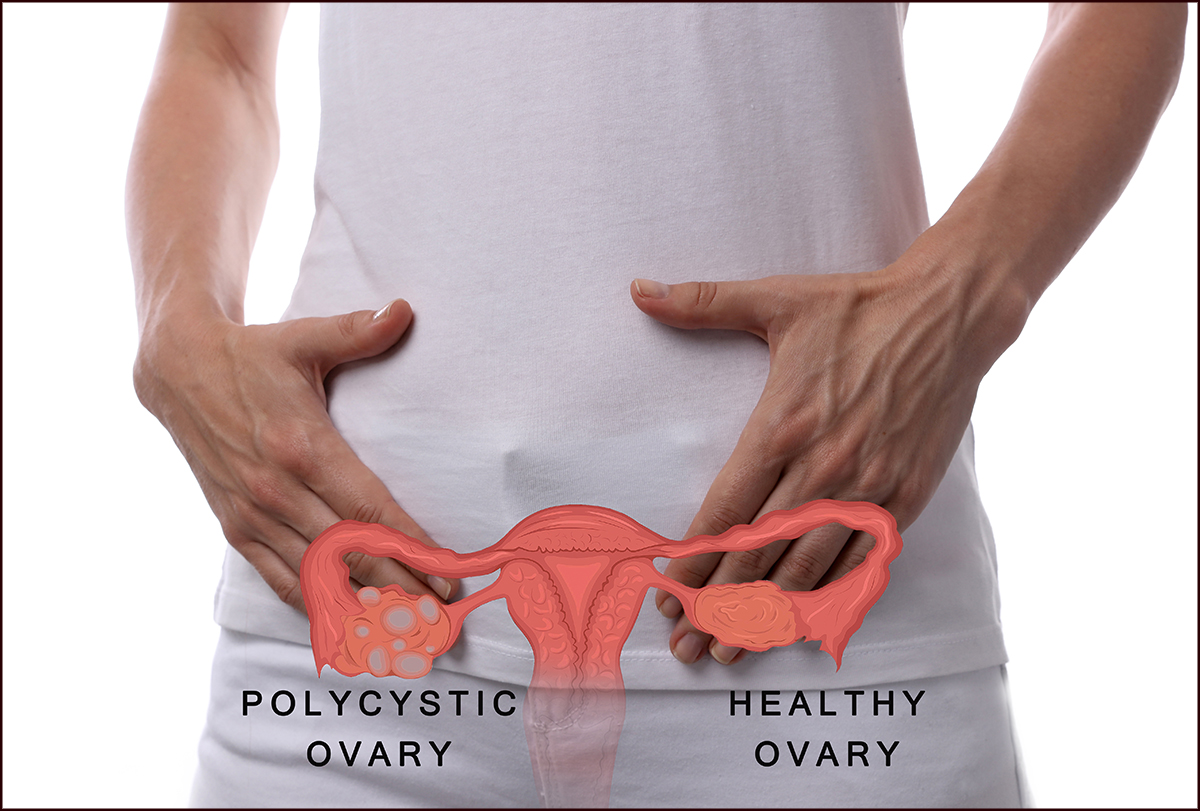
- In the majority of PCOS cases, one or both the ovaries sprout benign fluid-filled sacs or cysts.
- The excessive androgen secretion can lead to male-like features such as hirsutism, or the growth of extra unwanted hair on the face, chin, and other parts of the body where women typically do not have hair.
The signs and symptoms of PCOS vary from patient to patient. Some of the most commonly reported ones are:
- Hair loss from the scalp or male-pattern baldness (6)
- Excessive cramping and bloating during menstruation
- Skin that is greasier than normal, causing acne breakouts on the face, chest, and upper back
- Dark skin patches on the body, especially in areas with skin folds, such as the neck, groin, and under the breasts
- The appearance of skin tags, or small flaps of excess skin, in the armpits or around the neck
- Difficulty conceiving due to irregular ovulation or no ovulation at all
- Psychological stress and depression
- Fatigue and low energy for no discernible reason (other PCOS-related issues such as poor sleep may further aggravate the feeling of fatigue)
- Pelvic pain
- Rapid weight gain and difficulty shedding the extra kilos, making women with PCOS prone to obesity
- Increased susceptibility to mood swings, depression, and anxiety
PCOS can also lead to the onset of other chronic ailments over time. Women with this condition are at an increased risk of developing insulin resistance, type 2 diabetes, high blood pressure, high cholesterol, and heart disease. (7)
Early treatment and regular follow-ups can help safeguard you from these negative outcomes.
Medical Treatment

There is no absolute cure for PCOS. Hence, the primary aim of treatment is to manage the condition.
Several medical interventions can address the main symptomatic concerns associated with PCOS, which include hirsutism, acne, weight issues, menstrual irregularities, and infertility.
Managing hirsutism (excessive hair growth)
One of the most conspicuous ill effects of PCOS is hirsutism, or excessive hair growth on the face and the body. A couple of treatment techniques can address this problem:
- Removing hair: Facial hair removal creams, laser hair removal, and electrolysis help remove excess hair. While hair removal creams and products are readily available at drugstores, procedures such as laser hair removal or electrolysis require the expertise of a doctor and can only be performed clinically.
- Slowing hair growth: Your doctor may prescribe a skin treatment using eflornithine HCl cream to reduce the growth rate of unwanted facial or body hair.
Medication
Doctors routinely recommend the following medicines to manage PCOS symptoms:
- Hormonal birth control
- Anti-androgen medicines
- Metformin
- Statins
These drugs are attributed with anti-inflammatory properties that can help diminish certain inflammatory markers that are typically elevated in PCOS. (8)
How Is PCOS Diagnosed?
If your physician suspects that you have PCOS, he or she will most likely refer you to a gynecologist or an endocrinologist for a more thorough analysis.
For the diagnosis of PCOS, two of the following three are required:
- Irregular periods
- Excess body and facial hairs, acne, or blood tests indicating high levels of testosterone
- Ultrasound scan showing cysts on the ovaries
Based on these criteria, PCOS can be classified as mild, moderate, or severe.
Who Is at Greater Risk of PCOS?
According to a 2017 study, PCOS is more common among Middle Eastern women than among Caucasian females residing in the United States and Europe, but the highest incidence is reported among black women of African-American and Afro-Brazilian descent. (9)
Complications
Women with PCOS are increasingly prone to the following complications:
- Loss of fertility
- Insulin resistance
- Prediabetes/diabetes
- Elevated cholesterol levels
- High triglyceride levels
- Heart disease
- Stroke
- Endometrial cancer (cancer of the inner lining of the uterus)
- Obesity
- Sleep apnea
When to See a Doctor
It is well-advised to consult your healthcare provider for proper diagnosis and treatment if you are:
- Regularly missing your periods without being pregnant
- Concerned about symptoms such as hirsutism, acne, and male pattern baldness
- Unable to conceive despite repeated attempts
- Experiencing symptoms related to diabetes such as increased thirst, hunger, blurred vision, and sudden weight loss
Expert Answers (Q&A)
Answered by Dr. Harshal Deshmukh, MBBS, PhD (Endocrinologist)

In the short term, the answer is no. However, in the long term, women with PCOS have a significantly high risk of having obesity, diabetes, and other cardiovascular diseases such as coronary artery disease and stroke. (10)(11)(12)
Hence, PCOS can be life-threatening, and it is important to get the diagnosis as soon as possible and have a thorough long-term follow-up with an endocrinologist.
While there are no specific tests to predict which women with PCOS can become pregnant, usually those with mild and moderate PCOS are more likely to have a successful pregnancy.
A new test, the anti-mullerian hormone (AMH) test, can tell the number of functioning ovarian follicles in the ovaries of women with PCOS. Normal levels of this hormone mean a high chance of a successful pregnancy. (13)
Many women living with PCOS can also have a successful pregnancy using assisted reproductive technologies (ART) such as in-vitro fertilization.
Polycystic ovarian syndrome (PCOS) and polycystic ovarian disease (PCOD) are terms that are generally used interchangeably. PCOS is now the more accepted term as it reflects the complete spectrum of clinical and biochemical features of women living with PCOS.
Weight loss with dietary changes is the mainstay of PCOS management. A majority of women with PCOS have insulin resistance. Thus they need higher levels of insulin to keep their blood sugar level in a normal range. Insulin resistance also leads to obesity.
Hence, women suffering from PCOS should limit their intake of refined sugar and eat a low-carbohydrate diet. This means avoiding fizzy drinks and foods that have a high glycemic index, such as potatoes, rice, and white bread. It is important to work with a dietitian to have a dietary plan with a low-carbohydrate diet.
There is no cure for PCOS. However, a majority of PCOS symptoms can be reduced through weight loss. Once the diagnosis is made, weight loss is the mainstay of treatment.
There is a suggestion that if women with PCOS lose a sizeable amount of weight in the short term using a very low-calorie diet, some of the clinical and biochemical features of PCOS can be reversed.
PCOS is usually diagnosed when women recognize that their periods are irregular, they have excess body and facial hair, and they are unable to become pregnant. These features tend to stay constant during the lifetime of women with PCOS.
However, the metabolic features of PCOS, such as excess weight gain, high cholesterol levels, high blood sugars, and diabetes, worsen with old age.
Women with PCOS are also at an increased risk of cardiovascular diseases such as heart attack and stroke. Hence, they need regular follow-ups with their general physicians or endocrinologist to monitor these conditions.
Women with PCOS can have very heavy and painful periods. If this happens, it is important to consult your general physician or gynecologist. Some women with PCOS have no or only very few periods.
It is important that they have at least three to four periods in the year so that the endometrial lining is shed off. Generally, in women with PCOS, hormonal contraceptive pills are used to regulate periods and balance the hormones.
Here are a few things you can do to manage your PCOS symptoms:
– Make an effort to lose the excess weight by following a low-carbohydrate diet and exercising regularly.
– If you are planning to have a baby, see your endocrinologist as soon as possible. He/she will treat your PCOS and will rule out other conditions that mimic PCOS.
– Avoid smoking, excess alcohol, and things that increase your risk for cardiovascular disease as women with PCOS are already at a higher risk.
– Women living with PCOS are more likely to be depressed than women in the general population. Hence, it is important that you address your mental health. Yoga, meditation, and Pilates are very useful tools.
Final Word
PCOS is generally a lifelong condition that can best be managed rather than cured. Early diagnosis is crucial for reducing the severity and potential complications associated with this problem.
So, you must consult your doctor as soon as you suspect the first sign of PCOS. Based on a preliminary checkup, your physician may refer you to an endocrinologist for a thorough assessment. The specialist can then recommend suitable dietary, lifestyle, medicinal, and other therapeutic interventions to help you deal with this chronic problem.

- Was this article helpful?
- YES, THANKS!NOT REALLY


