In this article:
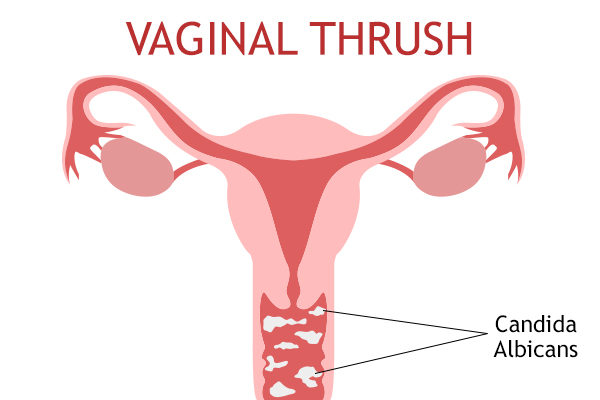
Thrush, medically known as vaginal candidiasis, is a common yeast infection of the vagina due to an overgrowth of Candida species. Vaginal thrush is also called moniliasis or candidal vulvovaginitis. The symptoms of vaginal thrush may cause vulval and vaginal pruritus/irritation and discomfort.

Candida species is identified in 10%–20% of healthy women in the reproductive age group, 6%–7% of menopausal women, and 3%–6% of prepubertal girls. (1)
Self-diagnosis of vulvovaginal candidiasis is frequently inaccurate and should be discouraged.
Causes of Vaginal Thrush
The chief cause of vaginal thrush is the overgrowth of Candida species that penetrates the superficial cells of the vagina. This yeast, along with certain species of bacteria, is part of the normal, healthy microflora of the intestines and vagina.
Generally, a healthy vagina maintains slightly acidic conditions through self-regulation, along with the help of good bacteria such as lactobacilli. The acidity keeps the yeast growth in check.
An imbalance in the good bacteria can result in a yeast infection or thrush.
Various risk factors for vaginal thrush include:
1. Antibiotics
Taking antibiotics may kill some good bacteria that keep the growth of Candida in check.
2. Hormones
Women are vulnerable to thrush outbreaks during their reproductive age (20–40 years), especially during puberty, ovulation, or menstruation. Pregnancy and postmenopausal estrogen therapy are also risk factors for vulvovaginal candidiasis due to the increased estrogen levels.
3. Contraceptive devices
Vaginal sponges, diaphragms, and intrauterine devices (IUDs) have been associated with vulvovaginal candidiasis, but not consistently.
4. Sexual behavior
An increased frequency of vulvovaginal candidiasis has been reported at the time most women begin regular sexual activity.
5. Immune response
A weak immune system, due to any illness (such as HIV) or medications (steroids and chemotherapy), is unable to fight an infection caused by Candida overgrowth.
6. Underlying conditions
Diabetes causes a rise in blood sugar levels, therefore increasing the risk of yeast infections. Iron deficiency can also contribute to thrush.
Symptoms of Vaginal Thrush
The symptoms associated with vaginal thrush vary widely. Some women do not experience any symptoms, whereas others may manifest the following:
- Thick yellow/white discharge with a cottage cheese appearance
- Itchiness or irritation around the vaginal and vulval area
- Inflammation in the vagina or vulva
- Stinging sensation while urinating
- Redness on the external skin of the vagina with a whitish coating
- Pain and discomfort during sexual intercourse
- Sores or cracks on vaginal skin
Medical Treatment for Vaginal Thrush

The standard treatment for mild cases of vaginal thrush involves the use of antifungal medications, which help reduce the symptoms in 1–2 weeks. These medications are available in different forms, including:
1. Intravaginal capsules
Pessaries are pills that are inserted into your vagina using a special applicator. It is important to use the applicator carefully, especially if you are pregnant.
2. Intravaginal creams
These creams are applied in and around the vagina using an applicator to help relieve the soreness and itchiness. The most common OTC creams include clotrimazole and miconazole nitrate.
3. Oral pills
The common antifungal capsules taken orally are fluconazole (prescription drug) and itraconazole (prescription drug).
In randomized trials, oral and topical drugs had similar clinical cure rates. Studies have shown that patients have reported a preference for oral treatment. (2) However, topical treatments may have side effects such as local burning or irritation, while oral medication may cause nausea, vomiting, diarrhea, headaches, rash, and transient liver function abnormalities.
In addition, oral medications take a day or two longer than topical therapy to relieve symptoms. For pregnant women with symptomatic Candida infection, topical clotrimazole, or miconazole vaginally for seven days, is recommended rather than treatment with oral fluconazole because of potential risks in pregnancy. (3)
Boric acid (600 mg boric acid intravaginal suppositories daily for 2 weeks) can be considered in cases of proven azole-resistant infection.
Diagnosing Vaginal Thrush
Vaginal thrush can be mistaken for a variety of other conditions that cause itching and redness, either with or without discharge. It is suggested to visit a medical professional if you notice any vaginal or vulvar irritation or abnormal discharge.
To diagnose the condition, the doctor will:
- Evaluate your symptoms
- Examine your genitals
- Take a vaginal swab for culture and microscopic examination
If your infection is recurrent, the doctor may also perform tests to rule out medical conditions such as HIV and diabetes.
Recurrent Vaginal Thrush
Vaginal thrush is considered to be recurrent when at least four discrete episodes occur in one year, or at least three episodes occur in one year and are not related to antibiotic therapy.
Recurrent candidiasis causes a burning sensation, inflammation, redness, irritation, and soreness in the vulvovaginal area. It may also cause vulval fissures (skin splitting) and extreme discomfort and pain during sex.
It is vital to get recurrent vulvovaginal candidiasis clinically evaluated to identify the underlying cause.
Complications of Vaginal Candidiasis
If left untreated for long, vaginal candidiasis may cause the following complications:
- Secondary infections
- Candida urinary tract infections due to spread of infection
- Chronic dermatosis and other skin conditions because of prolonged itching or infection
- Adverse pregnancy outcomes (4)
- Aggravated inflammation and other severe complications when accompanied by a weakened immune system
When to See a Doctor
It is recommended to see your gynecologist if:
- You are experiencing symptoms of thrush.
- The infection is recurrent (more than two episodes in 6 months).
- You are pregnant or breastfeeding.
- Over-the-counter treatment is not working.
- You have lowered immune strength due to conditions such as HIV and diabetes or chemotherapy.
Final Word
Vaginal thrush is an infection caused by an overgrowth of the yeast of the Candida species. This yeast exists naturally in the intestines and vagina. However, if there is increased growth, symptoms can develop.
See a doctor if your symptoms do not resolve with over-the-counter treatments. Follow preventive vulval hygiene.

- Was this article helpful?
- YES, THANKS!NOT REALLY


