In this article:
According to the American College of Obstetrics and Gynecology (ACOG), premenstrual syndrome (PMS) is characterized by physical or mood changes in women a few days before their period starts.

PMS symptoms can set in as early as 7–10 days prior to the start of menses and can persist for 1–3 days thereafter. The symptoms are repetitive and must occur for at least 3 months for the diagnosis to be made. (1)
PMS may be exhibited in one cycle and may not be present in the next. The severity of symptoms and occurrence may vary over the months and years and stop altogether after menopause. The association and prevalence of PMS cannot be predicted with respect to age, achievement, and social status. (2)
How Common Is PMS?
PMS affects nearly 12% of all females. Some women experience mild symptoms that are hardly a problem, whereas others have it far worse. In 20%–40% of PMS cases, the discomfort can be severe enough to hamper the woman’s productivity and quality of life. (3)
Causes of PMS
There is no clear reason for the occurrence of PMS, besides the sudden surge of the ovarian hormones in the female body 1 week prior to her period. This change may reflect upon the action of neurotransmitters, such as serotonin. However, it must be noticed that women with PMS may have a normal level of sex hormones.
Women who are highly prone to PMS-related discomfort may have low levels of serotonin and increased sensitivity toward the progesterone hormone.
But the exact risk factors that can increase one’s likelihood of experiencing frequent or intense PMS symptoms are not clearly understood and are subject to further investigation.
Signs and Symptoms of PMS
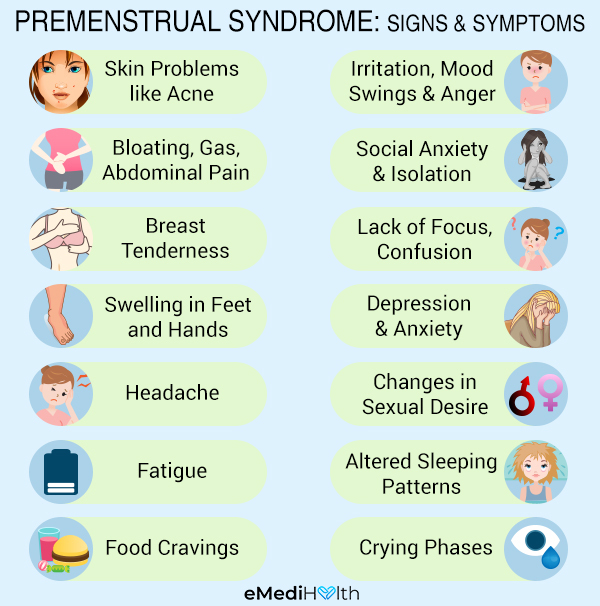
The physical symptoms of PMS include:
- Skin problems such as acne
- Bloating
- Gas
- Nausea
- Muscle cramps
- Breast tenderness
- Swelling in the feet and hands
- Headache
- Fatigue
- Excessive thirst
- Pelvic pain
- Stomach problems such as constipation
- Abdominal pain
- Back pain
- Diarrhea (in some cases)
- Water retention
The emotional symptoms of PMS include:
- Irritation
- Mood swings
- Social anxiety and isolation
- Difficulty concentrating
- Depression
- Frequent spells of anger
- Changes in sexual desire
- Altered sleeping patterns, either excessive sleep or a lack of sleep
- Crying phases
- Confusion
- Anxiety
- Food cravings
- Loss or increase in appetite
Medical Treatment for PMS

PMS treatment aims to address the hormonal activity within the body through hormonal or non-hormonal interventions for symptomatic relief. The doctor will recommend the ideal treatment option depending upon the patient’s condition, but some of the most commonly used ones include:
- Birth control pills or hormonal patches for women suffering from severe PMS or premenstrual dysphoric disorder (PMDD) to lower the hormonal levels.
- Antidepressants for women experiencing extreme emotional symptoms. These include selective serotonin reuptake inhibitors (SSRIs) and serotonin-noradrenaline reuptake inhibitors (SNRIs), which can help curb the depression and other psychiatric symptoms of PMS or PMDD. These must be prescribed by a healthcare professional.
- Nonsteroidal anti-inflammatory drugs to reduce pain. Although this area lacks research, a few pain-relieving medications can help reduce the characteristic spasms in the abdomen during PMS.
- Diuretics to prevent water retention in women experiencing a bout of bloating.
Note:
- Because antidepressants affect the number of neurotransmitters that are responsible for the generation of pain, it is necessary to take them only when you experience severe symptoms.
- The prescribed medications may have possible side effects and need further validation; hence, take them only when the pain is severe and ceases to go.
- Talk to your doctor if you are planning a pregnancy.
Severe symptoms that last for days and disrupt your daily activities must be evaluated by a healthcare professional.
Diagnosing PMS
Identifying PMS is difficult because of the lack of specific diagnostic tests.
- The healthcare professional is likely to make you record your symptoms over two menstrual cycles and give a retrospective account of the same.
- Reviewing 2–3 months of symptoms in menstrual charts is key for the health care provider to assess if symptoms can be attributed to PMS or PMDD or not.
- If the symptoms recorded are inconclusive, your doctor may recommend gonadotrophin-releasing hormone (GnRH) analogues for 3 months to confirm the diagnosis. (4)
Risk Factors for PMS
Factors that may contribute to the appearance of PMS symptoms include:
- A diet that lacks essential nutrients
- Women between the ages of 25 and 40
- Overweight, obesity, and high BMI – Women who have a high BMI are more likely to experience PMS than a normal-weighing woman.
- Stress and depression
- Being physically weak
- Smoking – A woman who smokes has twice as much risk of experiencing severe PMS symptoms as a non smoking female.
- Genetic predisposition
- Environmental toxins
When to See a Doctor
Severe PMS symptoms can disrupt your daily activities and thereby hamper the overall quality of life.
Thus, if you experience extreme discomfort that is hard to manage, it is essential that you visit a gynecologist, nurse practitioner, physician assistant, or midwife for a proper medical evaluation.
Consult your doctor if:
- Self-help tips and home remedies do not seem to work for you.
- You have suicidal and self-harming thoughts.
- You feel increasingly sad and hopeless.
- The symptoms are so bad that they disrupt your routine activities.
- The symptoms exist even after the first few days of your periods.
Expert Answers (Q&A)
Answered by Dr. Shalanda Webb, MD (Obstetrician and Gynecologist)

PMS symptoms normally occur for several days to 2 weeks before your menses (period). The patient generally gets relief once her period starts. The timing varies with everyone. Other medical conditions, such as endometriosis and stress, affect the duration and severity of symptoms.
PMS and PMT are the same. PMT is a term used by the World Health Organization (WHO) in the past.
PMS prevalence is not related to age. Age has no relationship with PMS, even in menopause. Perimenopausal women report symptoms consistent in their twenties to thirties (bloating, breast tenderness, mood swings, etc.).
The symptoms in postmenopausal women generally are weight gain and mood swings. The severity is dependent on multiple factors regardless of age.
Depending on the severity, PMS can be treated conservatively or with medical management. However, more research is needed to prove the efficacy of natural supplements as a treatment option.
– Lifestyle changes can improve symptoms. Exercising (including walking, running, and swimming) and practicing relaxation techniques (such as yoga and meditation) for 30 minutes have proven to lessen symptoms.
– Eating complex carbohydrates, such as whole grains, helps improve cravings and mood swings. Bloating can be improved by reducing salt and sugar intake. Limiting caffeine and alcohol intake may reduce symptoms.
– The medical management of PMS includes over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) and Midol, which should be used with caution and only after consulting with your doctor.
Some people with moderate to severe symptoms may need prescribed medication such as birth control pills or high-dose NSAIDs. I recommend talking to your doctor about either of these methods.
Premenstrual dysphoric disorder (PMDD) is a severe type of PMS. According to multiple studies, 5%–8% of women are suffering from severe PMS that affects quality of life. (5)
Both PMS and PMDD have physical and emotional symptoms, but PMDD symptoms are more extreme and cause mood to change dramatically.
If your doctor suspects you have PMDD, you will likely be referred to a mental health professional who can help you cope with the emotional and psychological stress associated with this condition.
The physical or emotional symptoms generally affect your work, social life, and everyday functions. PMDD risk may be higher if you have a history of anxiety, depression, and other behavioral issues.
If you are suffering from PMS, you should consult your primary care physician or gynecologist. Your clinician will ensure that your symptoms are consistent with PMS and not another disease (endometriosis, PID, etc.).
People who suffer moderate to severe emotional distress may benefit from antidepressants or anti-anxiety medication.
Final Word
Premenstrual syndrome is a monthly occurrence in the lives of many females during their childbearing years.
Incorporating some lifestyle and dietary changes a week before your period will help diminish the intensity of PMS symptoms and allow you to perform your best even in those difficult days.

- Was this article helpful?
- YES, THANKS!NOT REALLY


