In this article:
Most women in the developed world will spend greater than a third of their lifespan in menopause.

No wonder then that the symptoms that accompany menopause and the complications associated with aging have become increasingly relevant topics in women’s health today.
Fortunately, menopausal women now have multiple therapeutic options at their disposal to address legitimate concerns regarding their overall quality of life and general health.
What Is Menopause?
Menopause is the final stage of a woman’s reproductive life, which sets in gradually and not overnight.
Most women enter menopause in the latter part of their 40s or early 50s, which is characterized by the cessation of their menstrual cycle. In fact, a woman is said to have reached menopause if she goes a whole year without having a period.
As a woman ages, her ovarian function tends to decline gradually, until there comes a point when the ovaries stop producing certain hormones, specifically estrogen.
Since estrogen controls ovulation and menstruation, menopause marks the end of fertility for a woman. Simply put, a woman can no longer become pregnant after she crosses menopause.
The Age and Duration of Menopause
Fifty-one years is the average age when a woman stops menstruating. However, some can have an early onset of menopause at the age of 40 years or a late onset at 58–60 years.
Menopause is a natural transitory process that occurs over several years. A woman has to wait for a minimum period of 12 months since her last period to know that she is well into menopause.
Even after that, the symptoms tend to continue generally for 4–5 years but with reduced frequency and severity.
The Stages and Symptoms of Menopause
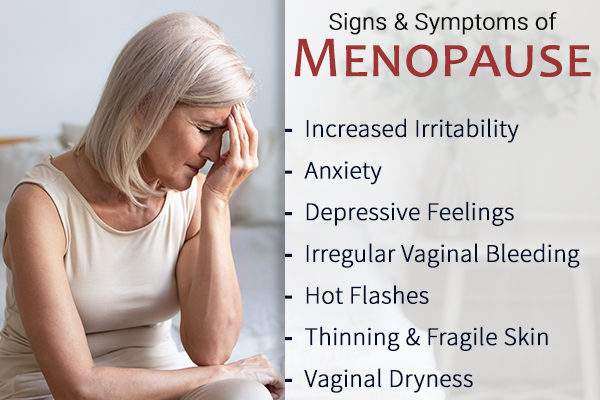
Menopause can manifest differently in different women. Some women have few or negligible symptoms, whereas others may experience increased irritability, anxiety and/or depressive symptoms, irregular vaginal bleeding (e.g., spotting), hot flashes, fragility and reduced elasticity of the skin, and some degree of vaginal dryness.
There are different stages of menopause. The first stage is previously termed “perimenopause,” now called “the menopausal transition,” which progresses to “menopause.”
The menopausal transition is the period when estrogen production by the ovaries fluctuates. Also, in this stage, the symptoms occur irregularly and unexpectedly, which can be quite frustrating.
Once menstruation abates for a total of 12 months, this is now termed menopause. The symptoms of menopause may still occur during this time but tend to lessen in intensity and frequency.
The Causes of Menopause
Menopause is considered a natural part of aging. However, if menopause occurs before the age of 40, termed premature menopause, it is usually an autoimmune process.
Health effects of this may be the earlier onset of disruptive symptoms, such as insomnia, vaginal dryness, hot flashes, and increased risk of bone loss.
Are Alternative Therapies and Home Remedies Safe?
People often opt for plant estrogens and herbal supplements over hormonal therapy since they are “natural,” which presumably makes them seem safer. However, this claim lacks scientific support and needs to be investigated further before these so-called “natural” alternatives can be advocated for large-scale use. (1)
You must consult your doctor before you start any such treatment as it can interfere with the medicines you are already taking and may not be as safe as once believed. (1)
Post-Menopausal Care to Avoid Complications
Some studies suggest estrogen helps prevent heart disease, which is the leading cause of death in women.
During menopause, estrogen levels are diminishing. So, you should try and lead as healthy a lifestyle as possible, exercise, and eat a healthy diet.
Osteoporosis is yet another major health threat for postmenopausal women, which can be averted by taking enough calcium and vitamin D every day. This condition is marked by a progressive loss of bone density, which renders your skeletal frame increasingly weak and brittle.
Doctors typically assess bone density through a test that gauges the strength of your spinal and hip bones. The results of this test determine the calcium and vitamin D dosage appropriate for you.
Women who are approaching or going through menopause can benefit a lot by staying physically active in terms of better health and reduced symptomatic discomfort.
Come up with an eclectic workout routine that includes both strength training and light weight-bearing exercises, such as walking and jogging, and follow it regularly.
Hormone Replacement Therapy for Better Heart Health
Hormone therapy has been the mainstay treatment for relieving postmenopausal symptoms for quite some time. It is also thought to reduce the risk of heart disease.
But does this claim hold any water when subjected to scientific scrutiny? Let’s find out.
Women tend to have a lower risk of heart disease than men but things change after they enter the menopausal transition.
With advancing age, women undergo a decline in their ovarian function, resulting in lesser and lesser estrogen production overtime. The drop in estrogen levels, in turn, increases the risk of heart disease.
For the past 20 years, doctors have routinely prescribed estrogen and other hormones to older women to safeguard their heart health.
However, recent studies to verify the cardiovascular benefits of hormone therapy have yielded mixed results, with a considerable number of women failing to register any significant improvement in their condition. (2)
The most extensive randomized, controlled trial conducted on the topic found that postmenopausal women using hormone therapy actually showed an insignificant increase in their heart risk, a claim which was corroborated by other studies as well. (2)(3)
There is, however, substantial evidence to suggest that the best time to undergo hormone therapy in order to derive its suggested cardiovascular benefits is when a woman is nearing the onset of menopause. (4)
As of yet, the relationship of the duration of such therapy to cardiovascular health is yet unknown and requires further research.
As always, hormone therapy should be individualized based on each woman’s risk-benefit scenario. Doctors continue to recommend hormone therapy’s effectiveness in the relief of menopausal symptoms to improve quality of life.
Potential Risks of Hormone Therapy
Even though hormone therapy has emerged as a standard treatment for alleviating menopause symptoms, a lot of women have reservations about the same, given the increased risk of heart disease.
To reiterate, the associated risk is only marginal; however, it is still a cause of concern for many.
It is therefore recommended to discuss your concerns with your physician, who will help put your personal risk into perspective and suggest the appropriate course of action.
If you are in the initial phase of menopause and are experiencing hot flashes and other menopausal symptoms but are otherwise healthy, the benefits of hormone therapy are greater than any of its potential risks.
In short, this therapeutic intervention is a fairly safe and credible option if you are experiencing severe menopausal symptoms, especially if your personal cardiovascular risk is low.
Several factors can increase your likelihood of developing heart disease, including family history, personal medical history, and overall diet and lifestyle.
All these factors will be taken into account by your physician before deciding upon the suitability and safety of hormone therapy for your particular case.
The Best Type of Hormone Therapy
Vaginal dryness, painful intercourse, and associated symptoms commonly experienced during menopause are the result of declining estrogen levels, which have been successfully compensated through estrogen therapy.
When administered vaginally, only minimal amounts of the estrogen get absorbed into the bloodstream, which reduces the risk of potential side-effects.
Low-dose vaginal estrogen is generally preferred over oral or transdermal therapy, mostly in cases when hot flashes are not present and particularly for the treatment of urogenital atrophy.
This low-dose therapy has to be administered only once or twice weekly in any of the following ways:
- Inserting small tablets (Vagifem) into the vagina before bedtime two times a week
- Applying an estrogen cream (Estrace, Premarin) over the vagina
- Wearing a vaginal ring called Estring, which releases low doses of estradiol into the vagina every 3 months in a sustained but controlled manner
Unlike women who are using oral or transdermal estrogen products, those who are taking low-dose vaginal estrogen are not prescribed progestins along with it. If you notice any unusual vaginal bleeding during the therapy, consult your doctor immediately.
While it is true that taking estrogen through the vaginal route is considered the safest option, this therapy is not without risk. As pointed out by certain studies, small but measurable amounts of estrogen steroid hormone, or estradiol, are present in low-dose vaginal estrogen products. (5)
Exposure to even trace amounts of estradiol can add to the risk of women who are already predisposed to severe cardiovascular disease or breast cancer.
Thus, women who cannot risk even the slightest estrogen exposure should speak with their gynecologist before starting even low-dose estrogen therapy. They have to weigh the risks against the benefits to see if it is a viable choice.
Menopause and Lost Sexual Desire
Sexual desire refers to thoughts and fantasies about sexual matters, and nothing satisfying happens without such sexual desire.
For most women, sexual thoughts and fantasies during the reproductive years are a life highlight that defines interpersonal relationships and impacts self-esteem. Sexual desire is at the center of the human sexual cycle and is most natural.
Hypoactive sexual desire disorder (HSDD) is a common problem that increases with age in many otherwise confident and well-adjusted women.
HSDD adversely impacts life quality in subtle ways with emotional disturbances that extend into family life and the workplace. For some, it is a minor short-term problem, whereas, for others, it may be debilitating.
Complaints about lost sexual desire are most commonly heard from older women. However, women of all ages may suffer from this.
Many women are embarrassed to share this concern and are reluctant to even ask their physicians about it. That is why physicians need to ask about it first.
There is good news about HSDD. Women and their doctors now discuss it more frequently. HSDD has previously had a reputation for being intractable and difficult to treat. This has changed.
What Causes HSDD?
In older women, HSDD is often a result of or is aggravated by a hormone dysfunction involving androgens. With advancing age, the production of androgens, such as testosterone, falls to lifetime low levels. This condition is particularly a problem for women who have had their ovaries removed, usually as part of a hysterectomy.
For older women, it appears that androgens, particularly testosterone, even in modest (replacement) doses, are effective in restoring sexual desire.
Situational HSDD is a common subtype of HSDD that is brought on by the loss or death of an intimate partner, dysfunctional relationships, or financial problems. These depressing circumstances can have a negative bearing on sex drive.
Treatments for HSDD
Normal female sexual desire requires a safe environment, self-esteem, and an attractive and available partner.
If you suffer from depression-induced situational HSDD but are otherwise healthy with normal androgen levels, your best bet is to manage the adverse life events through a multidisciplinary approach, which includes counseling.
Overcoming depression and your adversities will automatically restore your sex drive. In situations where sexual desire is a chronic, long-term problem, major psychotherapy may be required.
For women who have a deficiency of androgens, testosterone is the most helpful. Natural testosterone can now be administered through the skin using gels and lotions prepared for physicians by compounding pharmacies. The ointment is rubbed into the skin like a moisturizer, once or twice a day.
After about 5 weeks, the symptoms are reassessed, and a blood test (testosterone level) is done to evaluate for improvement.
There is now much high-quality evidence to suggest that transdermal testosterone has been effective in improving the quality of sexual life for many women. (6)(7) What is important to understand is that HSSD is a widespread concern shared among women.
Patients who are concerned they may have issues with HSDD or other sexual problems should be encouraged to bring it up with their physicians, even when the visit is about another matter.
Final Word
The growing awareness around reproductive health has prompted women to seek medical help for their menopause symptoms.
Presently, a myriad of options are available to address the symptomatic distress associated with this phase, hormone therapy being the most popular one. In fact, hormone therapy is the only treatment for hot flashes that has been approved by the FDA.
However, there is no one-size-fits-all approach when deciding the best treatment for menopause symptoms. Speak with your doctor about the pros and cons of various treatment options, and then make an informed decision.
- Was this article helpful?
- YES, THANKS!NOT REALLY


