In this article:
Eczema is a common skin ailment characterized by an underlying inflammation that manifests in the form of redness, swelling, itchiness, and scaly rashes on the surface of the skin.

As of now, the condition has no permanent cure, but most cases can be managed through proper doctor-recommended treatment.
How Common Is Eczema?
Eczema is one of the most commonly reported skin conditions, both globally and in the United States. The widespread prevalence of eczema is evident from the fact that more than 3 million people are diagnosed with it annually. (1)
Eczema affects nearly 20% of children and 3% of adults in the United States. (2) Almost 50% of the children who suffer from eczema carry this problem in their adulthood.
Types of Eczema
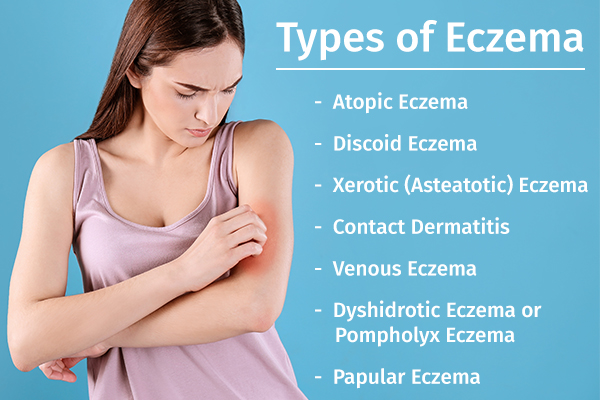
Eczema is an umbrella term for different types of eczema, all of which have certain distinguishing characteristics and result in the development of itchy, red, dry patches on the skin.
Here are some of the most prevalent forms of eczema:
1. Atopic dermatitis
Atopic dermatitis (AD), or atopic eczema, is a chronic form of eczema (3) that mostly targets the skin in the cheeks, neck, and limbs but spares the groin and armpits.
2. Discoid eczema
Discoid eczema is named so because it leads to the appearance of round or oval disc-shaped patches of red, inflamed skin. It is also known as “nummular” eczema (nummular means coin shaped).
3. Xerotic (asteatotic) eczema
Xerotic (asteatotic) eczema is a severe form of eczema that makes your skin extremely dry and inflamed, and the condition cannot be addressed through simple moisturizing but requires proper medical treatment.
4. Contact dermatitis
Contact dermatitis is characterized by skin irritation and itching (4) triggered by excessive contact with irritants (e.g., soap, detergents, harsh chemicals) and allergens (e.g., poison ivy, nickel, fragrances).
5. Venous eczema
Venous eczema, also known as gravitational dermatitis or venous stasis dermatitis, is a result of poor blood circulation in the lower legs.
The veins in the legs are fitted with valves that help push blood back to the heart. But the force of gravity plus the body weight puts extra strain on these valves, weakening them over time.
The damaged valves start leaking blood and fluid into the surrounding tissue, causing inflammation in the lower legs. This venous insufficiency and subsequent inflammation lead to the onset of eczema symptoms in the lower legs.
6. Dyshidrotic eczema or pompholyx eczema
Dyshidrotic eczema or pompholyx eczema is marked by the appearance of small but extremely itchy blisters on the palms, soles, and edges of the fingers and toes. (5)
7. Papular eczema (bumps)/eczema with follicular prominence
Papular eczema (bumps) and eczema with follicular prominence are rare forms of eczema that are typically observed in dark-skinned people.
Causes of Eczema
The exact cause of eczema is unknown, but it can be traced back to an overactive or highly sensitive immune system.
Various external and internal factors can trigger the immune system to produce an inflammatory response that targets the skin and results in eczema symptoms.
Some of the most common triggers for eczema flare-ups are:
- Stress
- Allergies
- Excessive sweating
- Irritants
- Sudden weather changes
- Extremely arid or hot and humid climates
- Hormonal fluctuations
- Certain soaps, cleaners, or detergents that remove the natural oils from the skin
- Long, hot baths or showers that dry out the skin
- Wool or man-made fabrics or clothing
- Environmental irritants such as dust or sand
- Tobacco smoke
- Foods such as eggs, milk, fish, soy, wheat, and nuts
- Bacterial skin infection or colonization
Symptoms of Eczema

Eczema can manifest differently in different people, but these are some of the commonly reported symptoms:
Eczema usually starts with the skin becoming red, itchy, and dry, which later turns into a rash. Constantly scratching the irritated skin can make it hard, thick, and dark.
The friction can even rupture your skin, resulting in an open wound that will most probably leave behind an ugly scar. These scars take forever to heal and may never go away completely. So, it’s best to resist scratching than regretting it later.
The symptoms and their location will mainly depend on the following factors:
- Age: Babies typically get eczema rashes on their face, torso, back, scalp, arms, and legs that may start off itchy but later become crusty or start oozing discharge. Adults usually develop eczema rashes on their face, wrists, hands, feet, and behind their knees. In older children and teenagers, the rashes mostly occur on the wrists, elbows, neck, and backside of their knees.
- Skin tone: Eczema patches look different in different skin tones. Light-skinned patients first experience skin redness that gradually turns brown. Dark-skinned people, on the other hand, may develop patches of lighter or darker skin in the affected areas of the body. This is because the underlying inflammation alters the function of melanocytes, which are skin cells responsible for producing melanin (the skin pigment).
- Type of eczema: Different types of eczema produce symptoms in different areas of the body at different times.
Medical Treatment for Eczema

Here are some of the commonly prescribed medical interventions for treating eczema and its scars:
1. Corticosteroids
Corticosteroids are often prescribed for both acute and chronic eczema to curb inflammation and therefore the severity of symptoms.
Most cases of eczema are managed through topical corticosteroids, but rare cases of severe discoid eczema may require oral steroids.
2. Immunomodulators
Immunomodulators help reduce skin inflammation by controlling the immune response responsible for it. This type of medication is found particularly effective against discoid eczema.
The doctor may prescribe azathioprine, dupilumab, methotrexate, or cyclosporine, which helps reduce inflammation by suppressing the immune system. (6)
3. Antihistamines
Antihistamines block the release of an inflammatory chemical called histamine in the body to ease eczema symptoms. This medication is primarily aimed at making the patient feel and sleep better, rather than curing the illness.
You must stick to the prescribed dosage to avoid oversedation, which can make you feel drowsy and dull for prolonged periods.
4. Antibiotics and antibacterial cleansers
Antibiotics and antibacterial cleansers are prescribed if the eczema rash gets secondarily infected.
5. Silicone gel technology
Silicone gel technology is the only topical treatment that has shown good results for flattening and fading eczema scars. (7)
You can use a Prosil Silicone Scar Stick to treat scarring on the exposed skin such as the face, neck, and arms, but silicone gel sheets are a better option for scars that remain covered by clothes.
6. Nonsteroidal creams
Nonsteroidal creams such as tacrolimus ointment or pimecrolimus cream may be prescribed by the dermatologist if all other treatments fail to bring down inflammation.
7. An emollient cream or ointment
An emollient cream or ointment helps moisturize the dry, scaly, eczema-ridden skin to make it less irritated and itchy. Moisturizing the skin religiously also helps strengthen its natural barrier function to prevent further damage or infections.
You must continue applying the emollient even after the rash clears and other medications have been stopped as part of your daily skin care routine.
In fact, the doctor may even recommend emollient soaps instead of the regular detergent-based soaps that can strip the moisture from your skin and make it even more irritated.
8. Clinical procedures
Clinical procedures such as dermabrasion, laser resurfacing, and ultraviolet light treatment may be recommended by your dermatologist to treat eczema scarring if topical ointments don’t work.
Diagnosing Eczema

Different types of eczema require their own specific treatment. Thus, your doctor will have to conduct a thorough examination to determine the specific form of eczema that is affecting you and then recommend the appropriate treatment. This involves the following steps.
- Direct physical examination of the affected skin
- Reviewing your medical history
- Inquiring about your symptoms, aggravating factors, and family history of eczema and associated diseases
If this preliminary investigation remains inconclusive, the doctor will order a few tests to reach a final diagnosis. These include:
- A skin biopsy, wherein a small sample of skin is cut out and examined under the microscope
- Patch tests, wherein possible allergens or irritants are applied to your skin to see if they trigger an inflammatory response
- Different types of allergy tests
- Skin scrapings, which are examined for signs of a fungal infection
- Skin swabs, which are tested for possible bacterial infections
When to See a Doctor
If you are affected by eczema, seek medical help if:
- Your skin becomes unbearably irritable, painful, and itchy.
- The itching and skin discomfort disturbs your sleep.
- The rash spreads to other areas.
- You notice signs of infection, such as yellow discharge or crusts on the affected skin or fever.
Final Word
The severity and duration of eczema can vary from patient to patient, but most cases are long-lasting, marked by periodic flare-ups.
Some people are lucky enough to experience only mild discomfort that subsides on its own or with minimal self-treatment. But those who suffer from persistent or extensive skin irritation will need medication along with proper diet, lifestyle changes, proper skin regimen, and self-care at home.
Untreated or poorly managed eczema can get progressively worse, but appropriate treatment can make the condition milder over time.

- Was this article helpful?
- YES, THANKS!NOT REALLY


