In this article:
When it comes to oral care, people usually focus most of their efforts on keeping their teeth healthy. The state of their gums or gingiva is usually neglected. A protective layer of gingival tissue covers the ultrasensitive dental roots (lower two-thirds of your teeth) and anchors your teeth in place.

Without the gingival tissue, the exposed dental roots will get damaged easily, and the tooth will eventually become unhinged.
What Is Gingivitis?
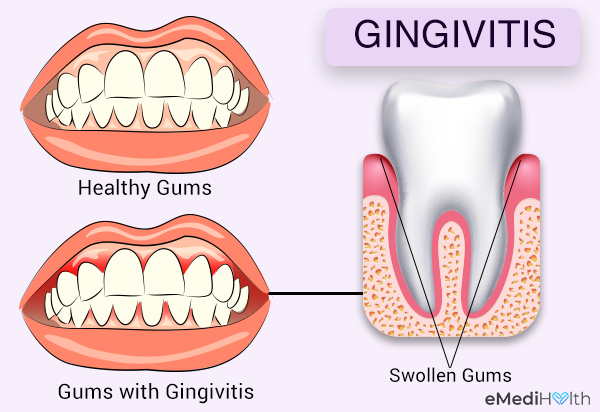
Gingivitis refers to the initial stage of gum disease that is characterized by inflammation or swelling of the gum tissue surrounding the teeth.
Negligent oral hygiene allows the bacteria in your mouth to flourish. These oral bacteria eventually settle on and around the teeth in the form of a sticky biofilm called plaque. The slimy coating of bacteria gradually hardens to form calculus, which stains your teeth and is hard to remove.
Types of Gingivitis
Gingivitis has two types:
1. Dental plaque-induced gingival disease
The most common culprit for gingivitis is dental plaque. If you do not clean your mouth adequately or regularly, oral bacteria multiply, eventually forming a sticky layer of plaque over the teeth and gums.
The gingival tissue becomes inflamed in response to the bacterial buildup and not due to any other local contributing factor.
2. Non-plaque-induced gingival lesions
Sometimes, the swelling in your gums can be traced back to factors other than oral plaque, including the following:
- An underlying systemic condition, such as an allergic reaction or certain ailments
- Certain pathologic changes in the gum tissues triggered by a specific microbial agent
- Genetic predisposition to forming gingival lesions
- Trauma or injury to the gingival lining
- A reaction to foreign bodies, such as dentures
- Idiopathic cause, which means you cannot pin the swelling on one specific cause (1)
Causes of Gingivitis
Generally, the causative factors of gingivitis are classified into primary and secondary factors.
1. Primary factors
The primary factor in most gingivitis cases is the accumulation of plaque and calculus with bacterial masses (associated with poor dental care). Plaque is an invisible sticky film of bacteria that can irritate your gum tissues and teeth.
2. Secondary factors
Secondary factors include cavities, broken teeth/fillings, ill-fitting dental prosthesis, smoking, stress, hormonal disturbances, and medical conditions compromising your immunity. A dentist will identify the specific factor for each case and then treat it accordingly.
Symptoms of Gingivitis
The symptoms associated with gingivitis include:

- Bleeding gums (the first visible sign of inflammation)
- Swollen, red gums
- Bad breath (also called halitosis)
- Receding gums and calculus buildup
- Gums that have pulled away from the teeth
- Gums that may be tender on brushing and flossing sometimes
- Swelling around a tooth
- Spacing and movement of teeth, called pathological migration (Spacing between teeth could be due to other reasons too.)
- Loose teeth
Dental Treatment for Gingivitis
The dentist will recommend the appropriate treatment based on the extent of damage and severity of your symptoms, but the most commonly used medical interventions for gingivitis include:
1. Antibiotics
Various antibiotic therapies can be used for gingivitis. Your doctor may write down a short course of antibiotic pills or capsules that have to be taken orally or recommend topical antiseptics to be applied directly to the gums.
Additionally, certain antibiotic solutions may be prescribed as a mouthwash to disinfect the oral cavity. However, antibiotic treatment may induce some side effects. Antibiotic pills, in particular, are known to trigger the following side effects in people with gingivitis:
- Digestive distress, which may lead to diarrhea
- Shortness of breath
- Facial puffiness or swelling
- Rash
- Bad taste in the mouth
2. Painkillers
If your gingivitis worsens or advances to a more severe form of gum infection, it may give rise to a considerable degree of pain.
Over-the-counter analgesics such as paracetamol and ibuprofen are effective for relieving mild pain, but it’s always better to consult your doctor about the appropriate drug and dosage instead of self-medicating.
Moreover, remember that pain medicine does not work as a standalone treatment for gum disease. It has to be used in conjunction with the doctor-prescribed antibiotics.
3. Anti-gingivitis toothpaste
Some of the active ingredients in toothpaste include amine alcohols, chlorhexidine, enzymes, herbal products, quaternary ammonium compounds, triclosan, zinc salts, and fluoride salts, which can help reduce gum swelling and plaque scores in your mouth when used regularly.
Fluoride toothpaste is considered to be the go-to oral hygiene product for preserving and improving periodontal health. But toothpaste that contains triclosan in addition to fluoride may provide a stronger cleaning action in reducing your plaque scores.
If you wish to prevent gingival inflammation and gingival bleeding, choose a toothpaste that contains not just one but both these protective agents. (2)
Toothpaste and dentifrices, when used on a toothbrush, are an ideal medium for these active components. They are effective in preventing plaque buildup in gingivitis if used for a long time. (3)
Diagnosing Gingivitis

Gingivitis is a gum disease and can only be properly diagnosed by a professional oral health care provider.
- A dentist conducts a detailed evaluation of your teeth and gums to check for tooth decay and plaque formation.
- The shape and color of the gingival tissue are examined on both sides of the tooth.
- The dentist records the amount of plaque and tartar on your teeth, swelling and inflammation of the gums, and presence of ulcers or abscesses.
- Teeth sensitivity would also be observed. The dentist will also check if there is mobility in your teeth to determine the bone loss.
- Dental X-rays help in the diagnosis when tooth decay is in its initial stages and has not resulted in oral cavities. They may also indicate how much of the gum is affected due to decay and if bone loss has taken place.
Depending upon the diagnosis, the ultimate treatment modality can be discussed with the individual.
Risk Factors for Gingivitis
Some factors can make you susceptible to gingivitis. These include:
- Crooked teeth that are difficult to clean
- Diabetes
- Excessive use of tobacco
- Genetic factors
- Low nutritional levels
- Obesity
- Taking certain medicinal drugs, such as antidepressants, heart ailment drugs, and birth control pills
- Hormonal fluctuations associated with pregnancy and the menstrual cycle and the use of oral contraceptive pills
- Old age
- Poor oral hygiene
Complications of Gingivitis
Gum disease that develops into periodontitis may lead to complications if left untreated. These complications include:
- Repeated formation of painful pockets of pus or gum abscesses
- Recession of the gumline due to prolonged damage to the gingival tissue
- Long-term corrosion of the tooth enamel due to the action of the oral bacteria, weakening the tooth significantly as time passes
- A buildup of plaque on and around the tooth, which can severely damage the periodontal ligament that connects the tooth to the socket
- Bacteria infiltrating the gums and reaching the underlying alveolar bone that holds the tooth in its place, progressively weakening the skeletal foundation of the tooth
In rare cases, a poorly handled case of gingivitis can escalate to a painful bacterial infection known as trench mouth. This extreme form of gingivitis goes by several names, including trench mouth, Vincent angina, or acute necrotizing ulcerative gingivitis.
When to See a Doctor
The above-mentioned remedies are helpful in treating gingivitis to a considerable extent. However, medical assistance must be sought if the condition becomes severe and unmanageable.
Consult your doctor if:
- You feel a lot of pain and discomfort.
- Your symptoms do not get better.
- You have red, swollen gums, especially if you have not had a dental checkup and tooth cleaning in the last 6 months.
Expert Answers (Q&A)
Answered by Dr. Wessam Atteya, BDS, FRACDS (Dentist)

Yes, it is. However, all the contributing factors need to be controlled.
Healing time significantly depends on the severity of the case and the control of causative factors that initiated and aggravated it. With good oral hygiene and control of other contributing factors, gingivitis can heal rapidly within a few weeks.
The simple answer is yes. However, most forms of gingivitis are not communicable, except for those caused by viruses and some bacterial infections.
No. Gingivitis must be treated by removing the causes of the condition. Salt water can help as an additional measure in very limited cases.
Preventive tips for gingivitis include:
– Brush your teeth at least two times daily using a soft toothbrush. It is recommended to follow the Bass technique for brushing the teeth.
– Floss daily.
– Visit your dentist regularly for professional checkups and cleaning.
– Avoid smoking.
– Control stresses and manage grinding/clenching.
– Eat healthy, well-balanced foods.
Available treatment options:
– See your dentist for a proper diagnosis of the contributing factor and follow their advice.
– Follow the preventative measures mentioned above.
Final Word
Practicing a complete oral hygiene routine can help you deal with gingivitis. It consists of brushing your teeth two times daily with a soft brush, rinsing your mouth with a mouthwash, and flossing adequately.
It is recommended to visit your dentist at least twice a year for a thorough dental checkup and professional teeth cleaning if needed. After assessing your oral cavity, your dentist may suggest additional oral health measures to remove the plaque and tartar from your teeth and gums.
Early treatment of gingivitis is the only way to avoid serious complications and irreversible periodontal damage.

- Was this article helpful?
- YES, THANKS!NOT REALLY



