In this article:
A sensation of pain or uneasiness in the head is termed as a headache. Headaches can occur in different areas of the head and can vary in intensity.

They can be triggered by a whole range of contributing factors and usually subside with proper rest. A headache may affect one or both sides of the head. It can be minor or chronic.
While most headaches are generally not indicative of a life-threatening medical condition, they do have an effect on daily life.
How Common Are Headaches?
The incidence of headaches increases when you enter your twenties. The rate of occurrence of headaches steadies by the time you reach the age of 40–50 and decreases after that.
According to the World Health Organization, around 50% of adults worldwide will experience at least one headache a year. (1)
Types of Headache
Headaches can be broadly classified into primary headaches and secondary headaches.
1. Primary headache
Primary headaches are not caused by any underlying medical problem but occur independently. These include:
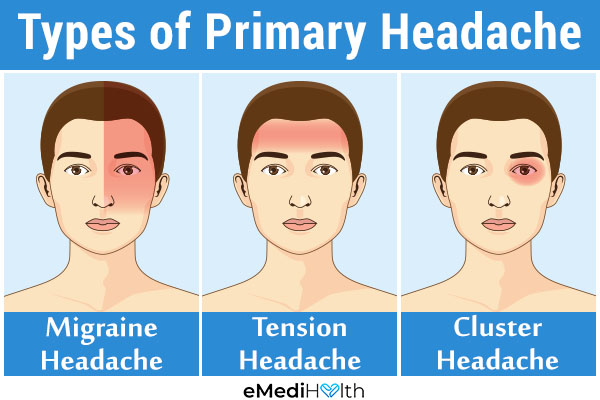
a. Migraine
During a bout of migraine, you may experience vomiting, photophobia (sensitivity to light), and lightheadedness along with a throbbing pain on only one side of the head.
b. Tension headache
More than 70% of adults suffer from tension headaches. These headaches are characterized by pain in both sides of the head, resulting in a tightening sensation.
They can occur frequently and continue for a few minutes or even days. Tension headaches can result from a bad posture or excessive stress. (1)
c. Cluster headache
This is the rarest form of primary headaches wherein you experience severe headaches that last for short durations but occur multiple times in a day.
Cluster headaches affect only 1 in 1,000 adults, mostly those above the age of 20. These headaches are generally focused around one eye. They can cause reddening in the eye, a drooping eyelid, and a runny nose.
2. Secondary headache
Secondary headaches result from an underlying disease or head injury that causes pressure on or displacement of pain-sensitive nerve endings. Thus, the pain occurs in parts of the head that have pain-sensitive nerve endings or muscles.
The brain tissue lacks such nerve fibers. Pain, signaled by tissues surrounding the brain, blood vessels in the skull region, and some nerves originating in the brain, can present as a headache.
Sinus problems, dental problems, and tension in the muscles of the neck and scalp can also cause headaches.
Causes of secondary headache include:
- Crying for a long time
- Genetics (migraine headaches can be hereditary)
- Stress and tension
- Dehydration
- Extreme cold or hot temperature
- Eyestrain (looking at the television, computer, or mobile screens for long durations)
- Strain in the neck
- Carbon monoxide poisoning
- Concussion
- Altitude sickness (lack of oxygen)
- Hormonal imbalance
- Using tight goggles
- Medication overuse
- Side effects of medication
- Hunger
- Excessive smoking or drinking
Medical Treatment for Headaches

The treatment for a headache depends on its type and cause. Maintaining a headache journal can help you in determining the reason behind your headache. Headaches caused by dehydration or a stiff neck can be avoided by making changes in your lifestyle.
Over-the-counter medications such as paracetamol/acetaminophen and ibuprofen can be used to relieve headaches. It is important to read the labels properly and not overuse the medications.
If you need to use over-the-counter medications for more than 2 days a week or if they fail to work, you should visit your doctor. He/she may prescribe you medications that are specific to migraines.
Note: Aspirin is not recommended for children and adolescents as it can cause Reye syndrome, which can be fatal.
Diagnosing a Headache
Different types of headaches produce different symptoms, which can help narrow down your diagnosis. If they point toward a primary headache, no further testing is required. However, if you have a secondary headache, further tests will help in determining the cause of your headache.
For better diagnosis, you can maintain a headache journal where you record the pattern, duration, and pain level of your headaches. This kind of in-depth information can help your doctor determine the type and triggers of your headache and thereby recommend the appropriate treatment plan.
When to See a Doctor
It is recommended to seek medical help when your headaches are highly recurrent or do not subside after using home remedies or OTCs. These headaches may indicate a severe medical problem.
Consult your doctor if your headache is associated with any of the following problems:
- Seizures
- Injury
- Fever
- Vomiting
- Changes in vision or speech
- Loss of motor function
- Numbness
- Stiffness in the neck
- Fainting
- Weight loss
You should seek medical help if you observe a change in the pattern or intensity of your headaches. Get regular follow-ups for the management of your headache if you suffer from an immune disorder or cancer.
Expert Answers (Q&A)
Answered by Dr. Ramon Rodriguez, MD (Neurologist)

Headaches are very common, and while most headaches do not have major implications and are benign, the presence of fever, chills, nausea, vomiting, changes in vision, weakness, or changes in body sensations could suggest a serious headache.
In such cases, I recommend a patient to have an MRI of the brain to assess in detail whether there might be any changes consistent with inflammatory disorders in the brain or brain vessels.
Another headache that can be serious is any headache in a person older than 50 years with no previous history of headaches.
Yes, hormonal changes can be associated with headaches. Fluctuating levels of hormones, such as estrogens and progesterone, may trigger headaches in females.
Another headache that can be attributed to hormonal imbalance is catamenial migraine, defined as migraine headaches that can begin 2–3 days before the onset of the menstrual cycle and may last up to three days after the menstrual cycle.
Paying careful attention to the cyclic nature of the symptoms can help with the diagnosis.
This is a very interesting question. Let’s begin with high blood pressure headache. While headaches are not a typical manifestation of high blood pressure, a headache that occurs secondary to high blood pressure raises the concern for malignant hypertension.
Elevated blood pressure might be associated with other conditions such as heart attacks or strokes, besides headaches.
Low blood pressures are typically not associated with headaches but can be associated with dizziness, especially upon standing and possibly fainting.
Migraines are more common than what people tend to believe. The typical migraine headache has three phases.
The first phase is the premonitory phase, wherein the patient feels they are going to have a “migraine or headache day.” It sometimes consists of changes in mood or irritability.
Then, the painful phase occurs, where the headache is typically unilateral, throbbing, behind the eye, and associated with nausea, vomiting, sensitivity to light or sound. The patient typically prefers to stay in a dark room.
After the painful phase (headache) is over, patients may suffer a postdrome, which can be associated with fatigue and malaise even for a day or two after the resolution of the headache.
Some migraines can have a little variability from the description provided, but most of them are associated with it. A regular headache tends to be all over the head or may be triggered by muscle spasms.
I recommend an evaluation with a neurologist because advances in medicine have provided information about the triggers and etiologies of many headache syndromes, and proper assessment can help choose the correct treatment.
As strange as it may sound, when a person has a headache, it is not typically the brain that hurts but the vessels and muscles surrounding the brain that irritates the nerve terminals and this is what causes the pain.
Many theories exist about what causes it, including inflammation and dilation of the vessels.
It could be. A person with a headache that is not improving with medications and continues to persist must be evaluated to rule out a structural lesion such as a brain tumor or must be checked for other conditions that may cause either elevated or decreased intracranial pressure.
When a person suffers from headaches, the most important thing is to pay attention to triggers of headaches. Unfortunately, most people don’t pay attention to the particular situations that provoke a headache, and many times the solution to make the problem better is there itself.
For example, stress, sleep deprivation, hunger, certain smells, some medicines, and even certain foods might be a headache trigger. Frequently, avoiding exposure to these issues can be all that is needed.
When a headache occurs, try to position yourself in a dark room and be quiet and even try to take a nap. Sleep is one of the best treatments for headaches. Avoid stressors. I know this is easier to be said than done, but small changes may create a long-term impact.
Medications such as acetaminophen or ibuprofen can be good first choices. Keep a journal of the time you are having headaches and situation and things you believe can be the triggers, and share this information with your doctor. For those where a headache has a change in nature, brain imaging is advised.
Final Word
Everyone suffers from headaches occasionally which can be triggered by a variety of factors. This discomforting nuisance is rarely a cause for concern, but you must seek medical help if the problem becomes increasingly frequent, severe, persistent, or is accompanied by other worrying symptoms.
Moreover, different things work for different types of headaches so there’s no single standardized treatment. Instead, your doctor will first diagnose the root cause of your recurrent headaches and then try a variety of treatments to find the one that suits you the best.

- Was this article helpful?
- YES, THANKS!NOT REALLY


