In this article:
Diabetes mellitus is one of the prime causes of morbidity and mortality among millions of people across the globe.

Innately intertwined with the development of cardiovascular diseases, blindness, nerve damage, kidney damage, and brain dysfunction, diabetes is a present-day global health challenge.
Despite the advancement in medical sciences and the implementation of prevention strategies, the increase in the prevalence of diabetes is projected to be 54% in 2015–2030, with a 38% jump in the number of deaths annually. (1)
Diabetes and Rising Sugar Levels
The food you eat is broken down to produce energy in the form of glucose, which is transported to the cells after digestive absorption. Each and every cell in the body requires energy to retain its structural and functional aspects.
Diabetes is a condition where sugar levels may rise when the cells in the body are unable to take up glucose from the blood in an efficient manner or due to insulin deficiency.
Specialized cells in the pancreas, a flat organ present in the abdominal region, produce a hormone called insulin and secrete it directly into the blood. The insulin in the blood is required to assist the movement of glucose molecules from your bloodstream into the cells. Once the glucose reaches the cells, it can be either used up or stored according to the energy requirements of the cell.
Whenever there is a reduced secretion of the insulin hormone or the body is unable to use the insulin efficiently, blood sugar levels rise. This heightened increase in blood sugar level is the hallmark finding in diabetes and entails a risk of various complications in the affected individual.
Types and Causes of Diabetes
Diabetes can be categorized into the following types:
Type 1 diabetes
Type 1 diabetes occurs when the body is unable to produce sufficient amounts of insulin. This type of diabetes develops as a result of the damage to the pancreatic cells that produce the insulin hormone.
Insulin injections are administered to patients with type 1 diabetes to stabilize their sugar levels and are life-sustaining. (2) Previously referred to as juvenile diabetes, we now know that anyone from any age group can develop type 1 diabetes.
Type 2 diabetes
Type 2 diabetes is the most prevalent type of diabetes, accounting for approximately 90% of the cases. Type 2 diabetes is marked by the body’s reduced or poor response to insulin, called insulin resistance.
Although there is a continuous production of insulin, insulin resistance prevents the transport of glucose to the body cells. With time, the insulin production in type 2 diabetes reduces gradually, giving type 2 diabetes its progressive nature.
Type 2 diabetes can be managed by making lifestyle changes and following the standard medical treatment. Various lifestyle and genetic factors play an important role in the development of this type of disease. (3)
Gestational diabetes
Gestational diabetes may develop in some females during pregnancy. Although it usually tends to go away after the birth of the baby, having gestational diabetes increases the risk of type 2 diabetes at a later stage in life.
At times, a case of type 2 diabetes in a pregnant woman may be misdiagnosed as gestational diabetes. (3)
Prediabetes
Prediabetes is a metabolic state that precedes the diagnosis of diabetes and is noted by higher than normal fasting or post-meal blood sugar levels. Having prediabetes puts you at great risk of developing diabetes in the near future. At this stage, there are interventions that can help you prevent the development of diabetes and is a call to action to maintain health.
Risk factors that have been associated with the development of diabetes include:
- Genetics/family history
- History of gestational diabetes or having a baby that weighs >9 lbs
- A sedentary lifestyle
- Being overweight or obese
- Being on medications that may inflict a harmful effect on the pancreatic cells that produce insulin, such as diuretics, antirejection medications, drugs to treat inflammatory diseases, psychiatric problems, and seizures, to name a few.
Signs of Diabetes
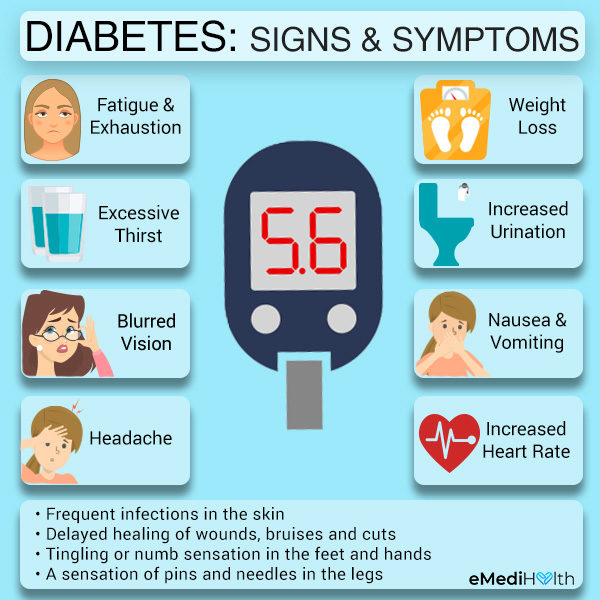
The appearance of the following symptoms can identify the presence of diabetes in your system:
- Fatigue and exhaustion
- Weight loss (despite eating your normal diet)
- Excessive thirst and dryness in the mouth
- Increased urination
- Blurred vision
- Feeling low on energy
- Nausea and vomiting
- Headache
- Increased heart rate
Individuals with type 2 diabetes may experience some other symptoms that include:
- Frequent infections in the skin
- Delayed healing of wounds, bruises, and cuts
- Tingling or numbing sensation in the feet and hands
- A sensation of pins and needles in the legs
Medical Treatment
Although diabetes remains an incurable disease, early type 2 diabetes can be managed and possibly reversed with changes in the diet and activity, improved sleep, stress management, and addressing other risk factors for complications.
This will require the patient to become educated and mindful about choices they make day to day. The purpose of medical treatment is to regulate the various parameters of blood glucose, blood pressure, cholesterol, and body weight.
The medically prescribed diabetes management involves the administration of oral medications, injectable medications, and insulin. When needed, your doctor may prescribe either of the following:
- Oral medications such as metformin that can help reduce the glucose levels or promote insulin function
- Injectable medications that are not insulin (GLP-1 agonists)
- Daily administration of insulin through syringes, pumps, and pen needles
- A cholesterol-lowering medication such as statin
- Medication to maintain normal blood pressure and to help protect your kidneys
Diagnosing Diabetes
A suspected case of diabetes can be confirmed through the following laboratory evaluations.
1. Fasting Plasma Glucose (FPG) Levels
The fasting plasma glucose test provides a measure of the blood sugar levels after fasting for 8 hours, usually taken early in the morning. An FPG test result of more than 126mg/dL on two or more occasions indicates that you have diabetes.
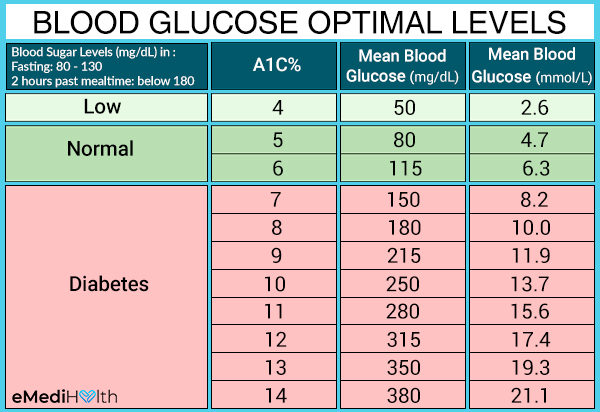
2. A1c Test (Hemoglobin A1C, or HbA1C)
The A1c test is a diagnostic test that determines your average blood glucose levels in the past few months. There is no need to do a fast for this test. It can also help previously diagnosed patients to determine if their treatment is working for them or not.
The results of the A1c test are given in percentage values. The higher the percentage of A1c, the higher is the measurement of the average glucose levels in your blood. An A1c level of >6.5% is indicative of diabetes.
3. Random Plasma Glucose (RPG) Test
This blood test is usually recommended when there are visible symptoms of diabetes present in the individual, and your doctor wants to get an immediate review. There is no need for overnight fasting for this test. Random blood glucose of >200 mg/dL is suggestive of diabetes and requires further testing.
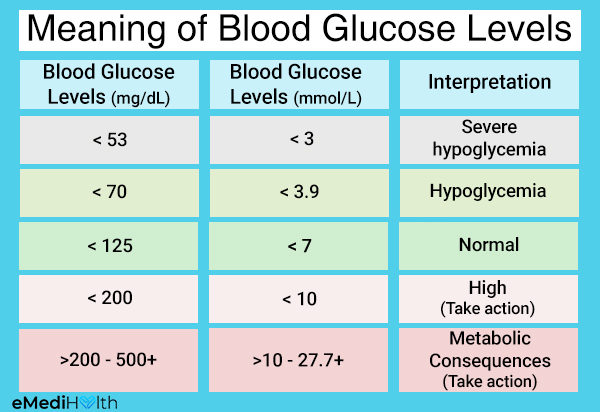
Blood Glucose Levels for People With Diabetes
Individuals with diabetes must keep tabs on their blood sugar levels in order to prevent complications. Based on large studies, keeping the blood sugar within the normal range can prevent the progression or development of complications.
With safety and prevention of low blood sugars in mind, it is recommended that individuals with diabetes maintain:
- A fasting blood sugar level of 80 to 130 mg/dL
- A 2-hour past mealtime blood sugar level below 180 mg/dL
Exceeding the 180 mark can lead to an accumulation of sugar in the blood and is known as hyperglycemia, while a sudden drop in your blood sugar level below the 70 mark is dangerous and is known as hypoglycemia.
- Whenever you experience a spike in your blood sugar levels, drinking1 – 2 glasses of water followed by a brisk walk can help bring it back to normal. However, if your blood exceeds the normal range more frequently for like three times in a span of 2 weeks, seek medical attention to optimize your diabetes management plan.
- Low blood sugar, or hypoglycemia, is a common occurrence in patients taking certain oral medications or insulin injections. The symptoms of hypoglycemia include feeling hungry, profuse sweating, and trembling. The recommendation for treating hypoglycemia is taking 15 g of glucose – you can have on hand glucose tablets or 4 oz of milk or fruit juices to raise your sugar levels. Meanwhile, keep checking your blood sugar every 15 minutes until it reaches >70. Depending on how low your blood sugar drops, you may find that you still have mild symptoms or fatigue despite the fact that your blood sugar levels have improved. Try not to consume too much to prevent rebounding high blood glucose.
Home Remedies and Tips to Manage Diabetes Naturally
There is no definitive cure for diabetes, but with your blood sugar levels under control, you can live a normal and healthy life. Various natural ways can be incorporated in your daily life that may help you control your blood sugar to an optimum level.
Here are some of the ways to control your blood sugar levels naturally.
1. Adopt changes in lifestyle and dietary patterns
Lifestyle changes can help manage diabetes to quite an extent.
These changes are focused on the elimination of activities that are potentially harmful to your health and replacing them with activities aimed at health promotion.
Altering your diet can help keep your blood sugar stable. Individuals diagnosed with diabetes are advised to become mindful of what they eat, to maintain proper portion sizes, and to restrict their consumption of foods that have a high glycemic index.
The glycemic index is a measure of the rapidity with which a particular food brings a surge in the blood sugar level. Avoiding processed foods and aiming for whole foods with lots of fiber some of the ways to simplify your meals.
The daily lifestyle and dietary interventions that are recommended for an individual diagnosed with diabetes include the following: (4)
- Restrict alcohol consumption to a minimum.
- If you are in the habit of smoking, quit it right away. Smokers are at a 50% greater risk of getting diabetes than non-smoking individuals and at a higher risk for complications.
- Aim for 7–8 hours of sound quality sleep.
- Limit your consumption of caffeine to not more than 4 cups a day.
- Monitor your blood sugar, weight, blood pressure, and cholesterol levels on a regular basis.
- Maintain a healthy body weight through a healthy diet and exercise. Start by asking your doctor what would be a healthy weight to strive for and set incremental goals to get there.
- Avoid deep-frying your foods. Include roasting, broiling, grilling, and barbequing in your culinary practices. Avoid sugary sauces by using fresh herbs and spices.
- Incorporate a large section of your diet with foods with a low glycemic index such as non-starchy vegetables including green beans, broccoli, cabbage, carrots, and cabbage.
- Limit your consumption of starchy foods with a high glycemic index such as pasta, noodles, bread, rice, processed oatmeal, white potatoes, sugary foods, and beverages.
- Reduce your intake of foods derived from animals such as poultry, eggs, red meat, and dairy. Choose lean meat, fish, tofu, and lentils as protein sources and pair them with lots of colorful vegetables. Consider switching to a vegan diet, even for just one day a week, to add abundant fiber and healthy carbs in your diet.
- Eat fiber-rich foods such as whole grains, colorful vegetables, and fruits such as blueberry, strawberry, apples. However, it is advised to eat fruits in moderation. Refrain from eating processed fats (trans-fats, interesterified fats, and margarine) Limit your salt intake. Choose expeller-pressed olive oil and incorporate healthy fats such as avocados, nuts, nut butter, flaxseeds and flaxseed oil, and chia seeds. Use stevia as a sugar substitute.
- Avoid using sauces, marinades, and dips that are high in fat and loaded with preservatives, additives, sugar, and salt.
- Vitamin D is positively associated with insulin production in the body. Spend some time daily in the sunlight to reap its benefits or take a supplement as recommended by your doctor.
- Keep yourself hydrated with water. Avoid sodas and packaged juice with added sugars.
- Individuals who cannot perform physical exercise may choose to work with a physical therapist to start from where they are and work on a graded exercise plan. This will help to avoid injuries.
- Stress may be the cause of your increased blood sugar level. Try relaxation techniques such as deep breathing and meditation or listen to soothing music to calm yourself. Have a daily practice of relaxation and perform mindfulness techniques throughout your day.
- Include a moderate quantity of white vinegar and apple cider vinegar in your meal preparations. Although vinegar consumption has been associated with considerable positive effects on diabetes markers, further studies are required to examine the long-term outcomes and the appropriate dosage of vinegar in type 2 diabetes. (5)(6)(7)(8)
- Add turmeric to your tea, milk, stews, or consume it as supplements. Turmeric is known to help fight oxidative stress, reduce the risk of dementia, decrease the rising sugar and lipid levels in the blood, which may eventually help curb the harmful effects of diabetes. However, further studies are required to determine the long-term use of turmeric as a remedy in affected individuals. (9)(10)
- Garlic can be added to your diet and has been shown to be effective for lowering blood glucose levels. Garlic extract is credited with a whole range of biological mechanisms that can prove beneficial for your overall health. The antimicrobial, prebiotic, anticarcinogenic, antimutagenic, antioxidant, immunomodulatory properties of this compound can be optimized for the management of diabetes in particular. The composition of garlic changes depending on how it is prepared. Garlic can be consumed raw or cooked, dehydrated garlic powder, garlic extract, or garlic oil prepared by an aqueous solution of garlic. Outside of adding garlic to your diet more scientific intervention is required to study the clinical use of garlic and its possible side effects. (11)(12)
- Some animal studies have backed the addition of okra to your diet with the intention to reduce glucose levels. Okra can be consumed whole, by roasting the seeds and soaked overnight to create okra water much like a tea. Okra has lots of properties in the form of vitamins and minerals; it is high in fiber and antioxidants. However, studies on human subjects are required to establish its beneficial effects and how it works to help manage diabetes. (13)(14)
- Using ginger medicinally has been shown effective in small randomized to improve fasting blood sugar and lower A1C. The dosage of ginger is important, and more research in human subjects is needed for a deeper understanding of its clinical use in individuals with diabetes. (15)(16)(17)
2. Engage in physical activity
Performing regular exercise can help stabilize sugar levels by enabling glucose uptake by the cells, thus lowering sugar levels in the blood.
Also, physical activity helps regulate various variables that are of utmost concern in the progression of diabetes, such as maintaining body weight and decreasing blood pressure, triglyceride, and blood sugar levels.
Following a regular exercise regimen also helps fight stress and improve the ratio of bad cholesterol to good cholesterol.
Engaging in physical activity curtails insulin resistance and reduces the risk of obesity/weight gain and cardiovascular complications that may arise as a result of uncontrolled diabetes. (4)
Incorporate an exercise regimen in your life for about 30 minutes every day at least 5 days week. You can also split it into a 10 – 15 minutes session two to three times a day.
- Brisk walking is a very easy way to stay active each day of your life.
- Engage in aerobic exercises such as dancing, aerobics, swimming, and cycling.
- You can also choose strength training exercises such as lifting weights to keep your muscles and bones strong and to keep a watch on your body weight.
- Perform stretching exercises to promote flexibility.
- Individuals diagnosed with prediabetes who exercise 150 minutes a week can reduce their chances of developing diabetes in the near future.
3. Consume fenugreek seeds
Fenugreek is a seed that has been used worldwide to aid in lowering blood sugar. Fenugreek seeds have been shown to stimulate the secretion of insulin in response to meals and to reduce the absorption of fat and glucose.
A bonus is that it is high in fiber, and it slows down the absorption of carbohydrates and sugars. (19) Several studies support the use of fenugreek seeds in regulating normal blood glucose levels. (26)(27)(28)
In a 2016 meta-analysis published in the Journal of Ethnopharmacology, fenugreek was included in the diet of 1173 subjects with diabetes type 2 and prediabetes, and it had favorable effects on fasting blood glucose, total cholesterol, and HbA1c. (19)
Another study found that consuming less than 2 grams of fenugreek was not associated with any prominent effects, while a dosage of 5 grams yielded significant positive results for the subjects. (25) However, some side effects were reported with the consumption of high dosages of fenugreek such as nausea, upset stomach, and odorous urine and sweat.
Caution:
- Pregnant women must refrain from the bulk consumption of fenugreek seeds due to the seeds’ ability to induce developmental abnormalities in the growing fetus. (45)
- Fenugreek can interact with blood thinners and cyclophosphamide.
- Do not take fenugreek if you have hormone-sensitive cancers such as breast cancer. (42)
- Consume fenugreek in moderation.
You can eat fenugreek seeds whole or grind the seeds into powder. It is best to add fenugreek seeds to your foods for a healthy diet plan. Fenugreek can be considered for its effects on lowering blood sugar, although it must be consumed in moderation to avoid any adverse effects on your health.
4. Eat bitter gourd (bitter melon)
Bitter gourd, also known as bitter melon, has been shown to have potential in lowering blood glucose in small clinical studies. It is known to influence glucose metabolism in the body, increase pancreatic insulin secretion, and affect insulin resistance.
A 2011 randomized control trial found that the treatment of 2000 mg/day of bitter gourd inpatients with type 2 diabetes resulted in a reduction of blood glucose levels. However, these effects were comparatively lower than those of the group receiving 1000 mg of metformin a day. (18)(22)
Another 2012 review that involved 479 patients found that there was no statistically significant improvement in the blood sugar level after consuming bitter gourd preparations for a period of 3 months. (44)
There were no side effects reported during the study.
Bitter melon can be consumed in several ways, including eating the melon, consuming the juice, or taking whole powder preparations, but there are no proven preparations to address diabetes specifically or independently.
Consider bitter melon if it is part of your ecology, part of your current diet, and something you enjoy. Do not consume it if you are pregnant.
Bitter gourd may play a role in diabetes management, but it should only be used as part of your healthy diet plan and an adjunct to the standard medications. Use caution when adding bitter melon to your diet, especially when you are taking medications for diabetes, as it may cause hypoglycemia.
5. Drink Aloe Vera Juice
Aloe vera contains phytosterols that possess possible antihyperglycemic effects in patients with type 2 diabetes.
A 2016 meta-analysis published in the Journal of Clinical Pharmacy and Therapeutics, which involved 470 patients with prediabetes and diabetes type 2, found that the supplementation of aloe vera juice led to improvements in the variables of fasting blood glucose and HbA1c. (34)
Aloe vera reduces the synthesis of glucose and the postprandial absorption of glucose in the stomach and intestinal region.
It is also suggested that aloe vera helps in the degradation of glucose and enhances its storage and expenditure. Although several studies reported that there were no side effects of aloe vera, there is a need for further research among large study groups. (34)(35)(36)
Aloe vera juice is made from the inner fillet of the leaf and can be consumed by adding its juice to smoothies, fruit juices, and regular water.
Aloe vera can be added to your healthy diet plan to help regulate your blood sugar levels. However, a more conclusive analysis is required to ascertain the efficacy of this remedy.
6. Include cinnamon in your diet
Fresh cinnamon contains bioactive components that may help reduce blood sugar levels.
A 2013 systematic review and meta-analysis published in the Annals of Family Medicine included 10 randomized control trials where the consumption of cinnamon was assessed in 543 patients. (29)
It was found that cinnamon intake significantly improved the levels of fasting blood glucose, bad cholesterol, triglyceride, and total cholesterol levels and increased the levels of good cholesterol at the same time.
A 2015 study published in Nutrition found that out of the seven clinical studies on cinnamon, five studies observed that cinnamon use was associated with a decrease in fasting blood sugar levels. (30)
However, the studies were conducted on a small group of healthy individuals, and this suggests a need for further research with people with diabetes and such that the results can be replicated.
Also, it must be noted that the commercially available cinnamon that goes by the scientific name of Cassia cinnamon contains an excess of the bioactive compound called coumarin, which if ingested in excess, can be toxic and can result in liver damage. (30)
A much safer option is the true cinnamon or Ceylon cinnamon, although considerable research is required to determine its effects on blood sugar levels. (30)
Cinnamon can be added to a variety of foods, desserts, salads, and teas/beverages.
Although cinnamon may help keep blood sugar levels stable, the lack of clarity regarding its use and the mixed reviews call for further scientific investigation to apply these results to patient care.
7. Consider powdered Indian gooseberry fruits
Indian gooseberry is rich in vitamin C, and its juice promotes the proper functioning of your pancreas.
The therapeutic use of this fruit is attributed to the presence of huge amounts of tannins that help increase the uptake of glucose. Gooseberry is also rich in minerals, namely, zinc, copper, and chromium. (21)
In addition to their blood sugar-lowering effects, the fruits of Indian gooseberry have been known to reduce the complications of diabetes on the eyes, heart, and kidneys. (24)
A 2011 study published in the International Journal of Food Sciences and Nutrition highlighted that consuming powdered amla fruits with water every morning resulted in a decrease in the levels of postprandial glucose and fasting blood glucose in individuals with and without diabetes. (20)
The study recommends further research to help confirm the use of gooseberry fruits as an alternative therapeutic cure for diabetes.
You may consume powdered gooseberry fruits with water.
Indian gooseberry is blessed with hypoglycemic properties, and further exploration is warranted to determine its exact mechanism of action in lowering blood sugar.
8. Use black cumin seeds
Black cumin is also one of the kitchen ingredients that may help you in managing your diabetes.
A 2015 study published in PLOS One reported that the consumption of black cumin every day as an adjunct was associated with better control on blood glucose and reduced levels of fasting blood glucose and HbA1c during the 1-year period of supplementation. (31)
A 2010 randomized control trial suggested that oral consumption of black cumin can help reduce the measurements of HbA1c, fasting blood glucose, and post-meal blood glucose levels in individuals with type 2 diabetes when taken along with the standard medications. (32)
Another 2016 review of 23 studies found that nearly 13 studies supported the positive effects of black cumin on lowering the fasting blood sugar. (33)
Add black cumin seeds or oil in your cooking preparations not only to enhance the flavor but also to reap the seeds’ benefits to your blood sugar levels.
Black cumin may be used as a complementary addition to the standard treatment to stabilize the blood glucose levels of patients with type 2 diabetes.
9. Take the recommended supplements
a. Chromium
Chromium is an element required by the body in very small amounts and is required for the metabolism of various biomolecules, including carbohydrates, proteins, and lipids.
Chromium deficiency was found in 31.5% of the participants in a 2014 study that included 108 individuals diagnosed with prediabetes. (23) Chromium deficiency may be present in diabetes patients.
Studies looking at the effects of chromium have conflicting results, and this warrants a more detailed evaluation of patient populations that may benefit from this mineral.
A 2014 study published in the Journal of Clinical Pharmacy and Therapeutics highlighted that supplementing chromium to patients with diabetes led to significant improvements in the levels of blood sugar, fasting blood glucose, HbA1c, good cholesterol, and triglycerides. (38)
However, an earlier study in 2010 demonstrated that chromium supplementation did not have a role in improving either blood glucose levels or insulin function. (37)
Chromium can be found in supplement form but should be taken with caution and never in excessive amount. Do not take it if you have liver or kidney disease.
Chromium can be added to your diet by consuming broccoli, barley, oats, green beans, tomatoes, romaine lettuce, and black pepper.
Chromium deficiency can be evaluated in people with diabetes and can be replaced if deficiency is discovered. However, the dearth of information in this regard calls for more rigorous studies to establish the exact relation between chromium deficiency and diabetes.
b. Magnesium
Magnesium is a mineral abundantly present in the body cells and is essentially present as an electrolyte.
An increased incidence of magnesium deficiency is found in individuals with diabetes type 2, particularly those with poor control on their blood glucose levels. (39)
A 2011 meta-analysis that included 536,318 subjects found that the risk of developing diabetes type 2 and magnesium intake are inversely related. (40)
Individuals with diabetes tend to have lower levels of magnesium than normal healthy individuals, which is attributed to either the increased urinary excretion or a comparatively lower dietary consumption of the mineral.
In a 2016 meta-analysis, oral administration of magnesium resulted in improvements in the fasting blood glucose in both patients with type 2 diabetes and high-risk individuals. (41)
You may add pumpkin seeds, spinach, Swiss chard, soybeans, sesame seeds, almonds, cashews, and bananas to your diet to up your magnesium intake. You may also ask your doctor for a supplement.
Although a deficiency of magnesium has been associated with diabetes, its role needs to be ascertained through large randomized clinical trials. Adding magnesium-rich foods to your diet will prevent the depletion of this mineral and must be part of a healthy diet plan.
Is Diabetes Reversible?
Although diabetes is considered an incurable disease, the scientific community is learning more and more about its reversibility.
Early diagnosis plays an essential role in diabetes management, and aggressive lifestyle changes can maintain your blood sugar levels within normal ranges without medication and can delay the progression of diabetes.
Although diabetes is usually categorized into type 1 or type 2, there is a lot of variability in the underlying defects that cause diabetes.
Hence, it is important to understand your case of diabetes, and the best management is designed by you and your doctor. Being an active participant in your health care decisions will serve you well.
The epidemic of type 2 diabetes is on the rise due to changes in our diets, the way we live our lives, and the natural cycles in our body and environment.
Addressing these key factors by taking prescribed medications if indicated, maintaining a healthy weight, getting quality sleep, regular exercise, and adopting healthy eating patterns will put you on the best path to good health.
If you have type 1 diabetes, type 2 diabetes for a prolonged period of time, or uncontrolled diabetes, there may be permanent damage to the pancreatic cells that produce insulin.
In such a case, you will have to depend on medications, including insulin to supplement your diet, and you need to exercise to keep your blood sugar levels stable and prevent any associated complications.
Who Are More at Risk?
Diabetes type 1 is likely to develop more in:
- Individuals who are genetically predisposed to the disease
- Children, teenagers, and young adults, although anybody can get type 1 diabetes at any age
Diabetes type 2 may develop if:
- You have been diagnosed with prediabetes.
- You are obese or overweight.
- You are 45 years old and above.
- You have a family history of type 2 diabetes.
- You have gestational diabetes or have given birth to a child weighing more than 9 pounds.
- You are of African-American, Hispanic/Latino-American, American-Indian, or Alaskan origin.
As diabetes can be inherited, children born to individuals with diabetes are at a greater risk of developing the disease.
Diabetes in children has been associated with a risk of damage to the heart, blood vessels, kidneys, eyes, and nerves, eventually leading to chronic health problems and even death in the early years of life.
Consequences of Diabetes
Elevated blood sugar levels for an extended period can cause a number of complications in the affected individual
These include:
- Cardiovascular problems affecting the heart and blood vessels. These may lead to coronary artery disease, heart attacks, peripheral vascular disease, and stroke.
- Kidney diseases as a result of the damage to blood vessels in the kidney affecting its normal function.
- Nerve damage can be induced by the toxic effects of high blood sugar, nerve compression, and lack of blood flow.
Neuropathy, or nerve damage, exhibits itself in the form of pain, a loss of sensation and tingling, most commonly affecting the peripheral body parts such as the hands and the feet.
More advanced nerve damage can affect gastric mobility, urination, blood pressure control, and heart rate. - Eye problems such as reduced vision or even blindness may occur if your blood sugar, cholesterol, and blood pressure are not regulated.
High-risk individuals are urged to get a diabetic eye screening examination done once a year to keep a check on their eye health. - Periodontitis may occur as a result of an increased risk of gum inflammation in affected individuals.
- Gestational pregnancy may increase the risk of the premature birth of the baby, increased birth weight of the baby, cesarean delivery, and preeclampsia.
Myths and Facts
Myth: Type 2 diabetes is a disease of obese and overweight individuals.
Fact: While obesity is a major risk factor for type 2 diabetes, obesity is not the only factor, and genetics play a role irrespective of the lack of any risk factors or a sound metabolic profile. (43)
It is important for you to understand your diabetes.
Myth: Eating too much sugar can cause diabetes
Fact: People often associate diabetes with excessive sugar intake. However, this is not true. Diabetes develops when your cells are not able to take up sugar, and there is a relative reduction of insulin secretion that cannot overcome the insulin resistance.
Excessive sugar intake is not recommended as part of a healthy diet and does play a role in the adverse metabolic effects and inflammatory nature of high-calorie, low-nutrient diets that damage your cellular response to insulin and the very cells that make insulin.
When you consume an excess of sugary foods, your body enters a phase where it converts the excess sugar to fats in the liver, leading to weight, obesity, and risk of developing type 2 diabetes.
So, it is best to restrict or at best avoid the consumption of sweetened foods and beverages. Individuals with diabetes need to eat a balanced diet with a low intake of sugar and consume foods high in fiber as directed by a dietitian.
Myth: Does everyone with diabetes needs to take insulin?
Fact: Because type 1 diabetes is an absolute loss of insulin, insulin administration must be taken to sustain life.
However, individuals with type 2 diabetes have a variety of medications available to them, including insulin, to optimize their blood sugar control and address the risks of complications.
Taking the prescribed medications and adopting a healthy lifestyle and diet may help regulate their blood sugar levels.
Myth: None of your family members have diabetes; that means you won’t get it.
Fact: Although family history is a risk factor when it comes to diabetes, an absence of the disease among family members only lowers your risk of getting the disease and does not completely eliminate it.
When to See a Doctor
Seek immediate medical help if you observe the appearance of the following symptoms:
- Persistent feeling of thirst
- Frequent urination particularly in the nighttime
- Feeling exhausted
- Losing weight without any effort
- Delayed healing of wounds
Final Thoughts
Statistics show a dramatic rise in the cases of diabetes and convey an alarming call to this global health problem, which needs to be addressed on a large scale.
You can help by taking care of yourself. Submitting to screening or diagnostic testing if you know you are at risk or you notice symptoms is of paramount importance when it comes to obtaining the best outcomes in diabetes management.
Although a chronic condition, diabetes can be managed largely by following a healthy diet plan, doing the exercise of your choice, taking the prescribed medical treatments, and keeping up with regular checkups to monitor your health status.
Be an active participant in your health care decisions and educate yourself often.
Expert Answers (Q&A)
Answered by Dr. Tharsan Sivakumar, MD (Endocrinology)
Both type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) have a genetic and environmental component. If both parents have T1DM, there is a higher likelihood that their child will develop it than if just one parent has diabetes. (46)
Furthermore, if one identical twin has T1DM, the other twin has about 50% chance of developing T1DM. (47) This suggests that there is about 50% contribution from genetics and 50% contribution from the environment for the development of T1DM. What those environmental factors are is still not fully understood.
With T2DM, if one identical twin develops T2DM, there is about 70% chance that the other twin will develop it. (48) Thus, the genetic component seems to be stronger in the case of T2DM than T1DM.
Diabetes is the number one cause of end-stage kidney disease in many developed nations. How rapidly diabetes causes damage to the kidneys depends upon genetic factors, the level of blood sugar control, blood pressure control, and the utilization of kidney protection medications.
On average, in T1DM, the prevalence of kidney damage (nephropathy) is about 6% after 1-3 years of having the disease. The prevalence reaches over 50% after having the disease for 20 years. With T2DM, up to 20% of people will have already experienced some amount of kidney damage at the time of diagnosis. (49)
There is ongoing research being conducted towards the goal of reversing diabetes-related kidney damage. For the most part, the damage to the kidneys is permanent, with only minor improvements being possible in most cases.
That being said, diabetes-related kidney damage can be slowed down by controlling blood sugar levels and blood pressure and by using medications that protect the kidneys.
There are different types of dementia, and diabetes has been associated with some types of them. Diabetes is most often associated with “vascular dementia,” which occurs because of reduced or blocked blood flow to parts of the brain, which is also the process that causes strokes.
People with diabetes have a higher chance of suffering from Alzheimer’s disease, as they too suffer from changes in the functioning of the brain. Drastic changes in brain functioning are some of the major characteristics of Alzheimer’s disease.
Diabetes has been associated with several mental health issues, including depression and anxiety. Studies have even found that diabetics are twice more likely to develop depression than nondiabetics.
However, it is also possible that people suffering from depression are more likely to develop diabetes, and thus it is difficult to determine which disorder caused the other. (50)
A silent heart attack means that the patient either does not feel any specific symptoms of the attack or simply does not recognize the symptoms as signs of a heart attack.
People living with diabetes are more likely to have a silent heart attack than those without diabetes. Further, women are more likely to develop a silent heart attack than men.
Otherwise, the risk factors for a silent heart attack are similar to those for a heart attack with symptoms including obesity, smoking, family history, age, high blood pressure, high cholesterol, and diabetes.
There are numerous risks of uncontrolled diabetes during pregnancy, including:
1) Large baby – The baby may have excessive weight at the time of birth (called macrosomia). Such babies are more difficult to deliver, are more likely to sustain birth injuries, and may lead to the requirement of a C-section.
2) Early (preterm birth) or miscarriage.
3) Respiratory distress syndrome – Breathing difficulties after birth, usually related to preterm birth.
4) Low blood sugar after the baby is born – This can sometimes lead to seizures in the newborn.
5) The baby has a higher chance of developing obesity and T2DM later in life.
Diabetes is a testing disease and poses many challenges. Nevertheless, it can be self-managed to some extent to keep it in check and also to reduce the risk of developing complications.
The following can help:
1) Lose weight: People’s blood glucose levels and insulin resistance will usually improve with weight loss, especially in people with T2DM.
2) Quit smoking: One should at least try to reduce the number of smokes per day if quitting is not possible immediately.
3) Exercise: Even a small amount of cardiovascular exercise can help with reducing blood sugar levels. Resistance exercise can also help to build muscle, which may improve insulin resistance as well.
4) Eat well-balanced meals: The focus should be on reducing carbohydrates, especially simple and processed carbohydrates, and reducing and eliminating fruit- and sugar-based juices.
5) Regularly follow up with healthcare providers: Detecting complications early allows one to take steps to mitigate the damage that diabetes is doing.
6) Check your blood sugars: This provides feedback as to how your lifestyle choices are affecting your sugar control.
7) Be informed: Learn as much as you can about how to manage diabetes, and have a discussion with your healthcare providers and other people living with diabetes.
About Dr. Tharsan Sivakumar, MD, FRCPC: Dr. Sivakumar is the Director of the Institute of Diabetes & Endocrinology, and the President-Elect of the AACE (American Association of Clinical Endocrinologists) Canadian Chapter.
He is board certified by the American Board of Internal Medicine in Endocrinology, Diabetes & Metabolism, as well as Internal Medicine. He is also a diplomate of the American Board of Clinical Lipidology.
In addition, he is certified by the Royal College of Physicians and Surgeons of Canada in Internal Medicine as well as Endocrinology and Metabolism.
His areas of clinical and research interest include diabetes, lipidology, and general endocrinology. He has a number of publications in prominent peer-reviewed medical journals.
- Was this article helpful?
- YES, THANKS!NOT REALLY


