In this article:
Hemorrhoids are lumps of tissue with blood vessels, muscles, and elastic fibers present in the anal passage. While most people think hemorrhoids are abnormal, the truth is everyone has them.

However, when the hemorrhoids surrounding the anal canal and the rectum become enlarged and engorged with blood, they cause symptoms. Enlarged hemorrhoids, also called piles, have caused millions of people discomfort, pain, and irritation.
Hemorrhoids are common and tend to occur more frequently in individuals between the ages of 45 and 65. As many as 75% of people in the United States have been affected by piles at some point in their lives. (1)
A case of hemorrhoids is not a very serious affair. They usually clear up on their own, but prolonged hemorrhoids accompanied with bleeding should be taken care of to avoid severe complications.
Fortunately, you can alleviate the symptoms of enlarged hemorrhoids by introducing some changes in your diet and lifestyle and trying out some simple and natural remedies.
Natural Ways to Cure Enlarged Hemorrhoids
Here are some home remedies for hemorrhoids.
1. Apply an ice pack

The first and foremost thing that you can vouch for to ease the inflammation and discomfort of piles is an ice pack. It is highly recommended to apply an ice pack on inflamed hemorrhoid.
An ice pack can successfully constrict the blood vessels, reduce swelling, and give you immediate relief from the associated pain.
The application of ice packs in combination with stool softeners and pain-relieving medications reportedly settled thrombosed prolapsed hemorrhoids in 10–14 days. (2)
How to use:
- Apply an ice pack or a partially melted piece of ice wrapped in a cloth directly on the affected area for about 10 minutes. Do this several times a day until the hemorrhoid goes away.
- You can even use a small pack of frozen vegetables such as peas or corn. Wrap it in a tea towel and then apply it on hemorrhoid, three times a day for 20 minutes.
2. Massage the area with aloe vera gel
Aloe vera is one of nature’s best ingredients for treating hemorrhoids. The anti-inflammatory and therapeutic properties of aloe vera help reduce the irritation and burning sensation induced by swollen hemorrhoid.
Aloe vera can be used for both internal and external hemorrhoids. (3)(4) A study corroborated the topical application of a cream containing 0.5% aloe vera juice powder as an effective treatment for chronic anal fissures. (5)
How to use:
To treat external hemorrhoids, apply a little bit of aloe vera gel directly to your anus and slowly massage the area. This simple remedy will alleviate your pain and soothe the burning sensation.
3. Take a sitz bath
A sitz bath is a warm water bath to relax the space between the rectum, buttocks, and hips.
Use a small bathtub and ensure your private parts are covered with water. A sitz bath can soothe the itching and inflammation around your anal region.
A sitz water bath twice a day for 10 minutes (no additives in the water) is helpful to patients with anal pain, itching, and burning. (6) Sitz baths have shown promising results on individuals with thrombosed hemorrhoids. (7)
Experts recommend a 20-minute sitz bath, two to three times a day, after every bowel movement. Gently pat the anal area dry afterward.
4. Increase your dietary fiber intake
Filling up on fibrous foods can bring regularity in your bowel movements. A healthy bowel function can help you prevent any future risks of piles.
Dietary fiber helps to create bulk in the intestine, which keeps your stools soft so that they can pass easily down the rectum and you do not have to strain during a bowel movement. (8)
A 2006 study published in the American Journal of Gastroenterology supported the consistent beneficial effects of fiber consumption in the treatment of symptomatic and bleeding hemorrhoids. (9)
Fiber-rich foods include:
- Fresh fruits such as pears, bananas, apples, raspberries, and figs
- Vegetables such as broccoli, green peas, and artichoke
- Whole grains such as oatmeal, brown rice, and barley
- Legumes such as beans and lentils
Note: Increase your fiber intake gradually to avoid gas, stomach cramps, and bloating.
5. Ease your bowel movements with psyllium husk
Commonly known as ispaghula, psyllium husk is a natural source of fiber prepared from the husks of the Plantago ovata plant’s seeds.
Psyllium husk is a supplement that provides necessary bulk to the food by soaking up water in your gut and forming a gel-like state to carry along the food through the digestive tract.
Hemorrhoid patients can vouch for the laxative properties of psyllium husk due to its role in improving bowel continence and promoting overall digestive health. (10)
Note: Make sure you drink plenty of water if you take this supplement.
6. Hydrate yourself with enough water

Adequate water intake is the most straightforward strategy to keep your digestive system running smoothly.
When suffering from either internal or external hemorrhoids, increase your water intake. Try to drink at least 8 to 10 glasses of water per day.
Adequate water intake helps clean your internal system and hydrates your entire body. It also facilitates bowel movements and keeps the stools soft, reducing the need for straining. (8)
When you don’t drink enough water and other fluids, the process of flushing out waste from the body slows down, and there can be a backlog in the bowel. The result is hard stools, which will worsen the problem of hemorrhoids.
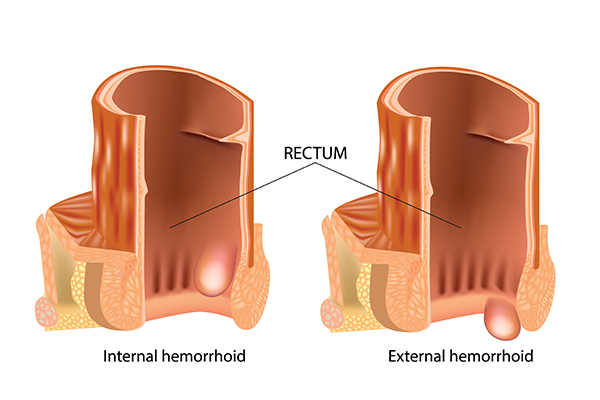
Types of Hemorrhoids
The type of hemorrhoids you have depends on where they occur.
1. Internal hemorrhoids
Internal hemorrhoids are located deep inside the rectum. They are not visible and cannot be felt. Internal hemorrhoids are accompanied by painless bleeding.
These painless swellings can be classified into four grades: (11)
- Grade 1 These hemorrhoids are found along the lining of the anus and cause no harm.
- Grade 2 These hemorrhoids are found along the lining of the anus. They pop out while passing stools and tend to go back afterward on their own.
- Grade 3 These are known as prolapsed hemorrhoids. Such hemorrhoids need a physical push by the patient to get back inside the anus.
- Grade 4 These hemorrhoids hang outside the anus and cannot be pushed inside forcefully. Grade 4 internal hemorrhoids can cause major discomfort due to the pain and swelling.
2. External hemorrhoids
External hemorrhoids are swellings that are located closer to your anus, marked by a supply of pain fibers. They are likely to be associated with pain and bleeding.
Causes of Hemorrhoids (Piles)
Enlarged hemorrhoids is a pretty run-of-the-mill medical condition that most of us dread.
They can result from an excessive strain on the blood vessels in and around the anus. This causes the anal tissue and blood vessels to become swollen and inflamed. The inflamed hemorrhoids can bleed, often during bowel movements.
Although there are certain causative factors that can lead to hemorrhoid problems, some people can develop hemorrhoids for unknown reasons. The following factors can be the primary causes:
- Constipation
- Straining during bowel movements, due to the inability to defecate normally
- Restricted movement marked by constant periods of sitting or standing
- Physical labor such as lifting heavy objects that can put extra pressure on the pelvic region
- Persistent coughing
- Inadequate fiber and fluid intake
- Being obese or overweight
- Repeated sneezing
- Frequent diarrhea
- Anal intercourse
Signs and Symptoms of Hemorrhoids
Hemorrhoids may not always cause pain or discomfort. You might be unmindful of their presence as they get cleared up on their own. The symptoms that might occur include:
- Bleeding while passing stools
- Painful bowel movements
- Anal burning
- Itching and soreness around the anus
- Swelling around the anal region
- Mucus discharge from the anus
- Discomfort and an urge to defecate even right after visiting the toilet
- Hanging hemorrhoids that need to be pushed back using your fingers after a bowel movement
Treatment of Hemorrhoids
Hemorrhoids are most often linked to the inability to pass your stools. Ensuring a healthy bowel function is the key to treat and avoid piles. (12)
Medical treatment
Apart from the conventional remedies and lifestyle changes, perpetual cases of piles can be treated by the following:
- Astringent ointments to shrink the swollen hemorrhoid.
- Hemorrhoidectomy and hemorrhoidopexy to extract the enlarged hemorrhoids.
- Hemorrhoid surgery – This is recommended in cases where most treatments fail to respond. The most important factor to be considered for surgical removal is the severity of hemorrhoid.
Minimally invasive standard medical procedures:
- Rubber band ligation – This involves tying the enlarged hemorrhoid with a rubber band, which cuts off the blood supply to the hemorrhoid. Hemorrhoid will then shrivel and fall off in 2–10 days
- Sclerotherapy – This requires the administration of a shot of a chemical solution to shrink the hemorrhoid.
- Electrical coagulation – This involves burning the inflamed tissue using a laser or an infrared light.
The primary objective in treating hemorrhoids is alleviating the extra pressure on the pelvic floor that can disrupt healthy bowel continence.
A diet rich in fibrous foods such as vegetables, fruits, and cereals and an adequate amount of water will help in easing your bowel problems and mitigating the associated pain and discomfort.
Lifestyle Changes to Prevent Enlarged Hemorrhoids
Introducing some lifestyle changes can alleviate your bowel irregularities in general.
Once you have a normal bowel function, you eliminate the possibilities of aggravating your hemorrhoids or developing them in the first place.
These can include the following:
- Increase the amount of fiber in your diet gradually. Consume about 7–20 grams of fiber daily. Good sources of fiber include vegetables, fruits, whole grains, beans, legumes, seeds, oats, and broccoli. (12)
- Include plenty of fluids in your diet, particularly water, to keep your stools soft. Avoid caffeine and alcohol.
- Do not ignore your urge to pass stools. Delaying the first call can disrupt your normal bowel function.
- Avoid taking medicines such as codeine that can cause constipation as a side effect.
- Try to maintain a healthy body weight. Being overweight can cause inflammation in your anal region.
- Avoid a sedentary lifestyle. Follow an exercise regimen to keep your bowels running and prevent constipation.
Preventive Measures to Be Taken

To prevent hemorrhoids, it is important to practice good hygiene and healthy bowel habits. The following tips may help you with maintaining the same and mitigating the discomfort and pain associated with piles:
- First and foremost, keep your anal area clean as much as possible.
- Use moist wipes to clean the anal region after every bowel movement.
- Limit your time on the toilet seat.
- Do not exert too much pressure to force a bowel movement.
- When you feel the urge to defecate, go as soon as possible.
- Try a squatting position or level yourself up placing your feet on a stool when sitting on the pot for a bowel movement. This will facilitate a less strenuous bowel movement by changing the position of your anal canal.
- Improve your dietary fiber and fluid intake to avoid constipation.
Risk Factors: Who Is Most Likely to Suffer?
Some people are more likely to suffer from enlarged hemorrhoids due to various factors including the following.
- Genetic predisposition to piles, characterized by genetically weak rectal veins, weak rectal vein walls, or weak venous valves
- Chronic constipation
- Pregnancy, which can exert extra pressure on your pelvis
- Sedentary lifestyle
- Progressive age-related weakening (above the age of 50)
- Certain diseases, such as cirrhosis and inflammatory bowel diseases
Hemorrhoids Related Complications
Piles can rarely put you in a complicated situation but persistent or severe cases of piles may cause other problems, which include the following:
- Blood loss and anemia Bleeding from long-term hemorrhoids can cause blood loss and result in iron deficiency.
- Clotting in the blood vessels Hemorrhoids that prolapse can lose their blood supply when kept sticking out. This can cause the formation of blood clots (thrombosis), which can be very painful.
When to See a Doctor
Booking an appointment for a hemorrhoid case may sound embarrassing to you, and you might be reluctant just at the thought of it.
Piles usually go away on their own or by simple home remedies and over-the-counter treatments, but a prolonged case of piles needs to be addressed with a proper diagnosis.
- Check in with your doctor if you have persistent or severe symptoms, such as if your toilet paper is smudged with blood more than normal. You should always get your rectal bleeding checked.
- Your GP will ask for your medical history and perform a physical examination of your abdomen and anus. This might be uncomfortable but necessary to understand your condition. The doctor may also prescribe you some tests to evaluate your condition and rule out the possibility of any other anorectal problems, such as fissures and abscesses, or other serious diseases of the bowel and anus, such as colitis and bowel or rectal cancer.
- The doctor may also prescribe you sigmoidoscopy and anoscopy to get a clear view of the inside of your rectum and anus to diagnose any internal hemorrhoids if present.
Final Word
Incorporating fibrous foods, adequate amounts of water, and a few behavioral modifications in your lifestyle can help you maintain a healthy bowel function. A smooth bowel movement can necessarily help you to manage piles and support your anorectal health.
- Was this article helpful?
- YES, THANKS!NOT REALLY


