In this article:
Celiac disease, also known as gluten-sensitive enteropathy, is an autoimmune disease affecting the small intestine of approximately 1% of the global population. (1)

Gluten, a protein found in wheat, rye, and barley, triggers an immune response resulting in inflammation of the small intestine.
The disease tends to occur in people who have what is known as the human leukocyte antigen (HLA) DR3-DQ2 and/or DR4-DQ8 gene. Over 99% of patients diagnosed with celiac disease have one or both of these genes. (2)
The Damaging Effect of Celiac Disease on the Small Intestine
To understand celiac disease, it is important to understand the normal physiology of the small intestine.
The small intestine is approximately 20 feet in length, and its primary purpose is to absorb vitamins and nutrients from digested food. (3)
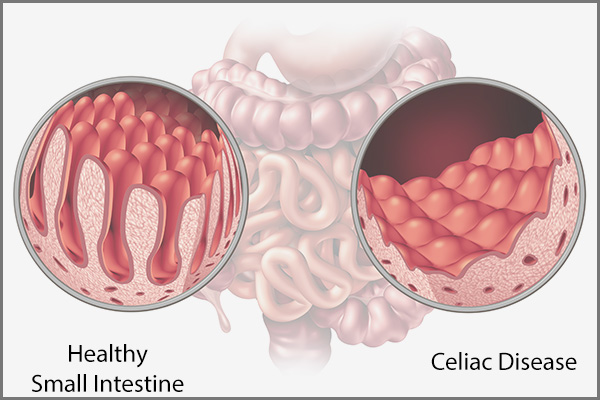
The inner lining (mucosa) of the small intestine has tiny hair-like projections called villi, which increase the overall surface area of the small intestine and, in turn, aid in the absorption of vitamins and nutrients.
When a person with celiac disease comes into contact with gluten, an inflammatory reaction occurs in the small intestinal mucosa, resulting in damage to the mucosa. This causes the villi to blunt, decreasing the surface area of the small intestine and hampering nutritional absorption from food.
Symptoms of Celiac Disease
Untreated celiac disease is associated with a decreased ability of the small intestine to absorb nutrients. Classically, symptoms include:
- Diarrhea, with large, foul-smelling, fatty or greasy-appearing stools
- Fatigue, which may be present due to iron deficiency anemia from impaired iron absorption
- Reduced sensation of touch due to impaired B12 absorption
- Osteopenia and osteoporosis, which may be complications of impaired calcium and vitamin D absorption
It is important to note that patients do not always present with textbook symptoms of the disease and may only experience:
- Recurrent, intermittent bouts of diarrhea
- Abdominal bloating
- Mild pain
In such cases, digestive distress can be wrongly attributed to gastritis, irritable bowel syndrome, or lactose intolerance, which present the same symptoms. For this reason, these people may remain misdiagnosed for years.
Diagnosing Celiac Disease
Celiac disease can be diagnosed using a combination of the following tests:
1. Serologic tests/blood work
Serum tissue transglutaminase (tTG)-IgA and endomysial (EMA)-IgA antibody tests both have similar sensitivity and high specificity for diagnosing the disease.
In patients at low risk for celiac disease, a negative serologic test essentially excludes the disease. However, if there are symptoms suggestive of celiac disease or if the serologic test is positive, then endoscopic evaluation is needed.
2. Endoscopic evaluation
An esophagogastroduodenoscopy (EGD) can be performed, which will show an abnormal appearance of the first portion of the small intestine, known as the duodenum.
Classically, duodenal “scalloping” is seen, along with the absence or blunting of duodenal villi. This can often be even better visualized using the water submersion technique.
3. Biopsies
This involves obtaining a small piece of the small intestine that is then evaluated by a pathologist to confirm the presence or absence of celiac disease.
Ways to Deal With Celiac Disease

Some of the most basic steps for managing celiac disease are:
- Exclude gluten from your diet completely, and consume gluten-free grains instead.
- Read the ingredient list of your food products for the presence of any trace of gluten before buying.
- Apply the same caution when eating out by categorically asking your waiter or food server about the ingredients used in your preferred dish before placing the order.
- Consume aloe vera juice regularly to soothe your digestive system.
- The impaired absorption of nutrients can render you increasingly deficient in vitamin D, which is why you must get enough sun exposure to help your body synthesize this key nutrient on its own.
- Eat a healthy, well-balanced diet that is rich in probiotics, fish oil, paprika, ginger, and blackstrap molasses to make up for the lack of nutrients.
Dietary Recommendations for People With Celiac Disease
Management of celiac disease is primarily dietary avoidance of gluten-containing products. This can be very challenging without precise guidance, so a registered dietitian should assist the gastroenterologist for a multidisciplinary approach to treatment.
The full list of items to avoid is beyond the scope of this article. However, it is important to know that the main sources of dietary gluten include wheat, rye, and barley. (4)
The Need for Nutrient Supplements
Supplementation with vitamins and micronutrients should only be done when clinically evident deficiencies exist.
However, certainly, when active, untreated celiac disease is present, vitamin D, calcium, iron, vitamin B12, and folate are frequently needed to be taken as supplements to replenish the body’s low levels.
Can Home Remedies Relieve Celiac Disease Symptoms?

Lastly, patients sometimes seek alternative or herbal medicines for assistance with their celiac disease symptoms. Unfortunately, evidence for products such as aloe vera and ginger is purely anecdotal at this time.
Lifestyle Changes to Manage Celiac Disease
Besides a gluten-free diet, adjunctive treatment can include lifestyle modifications. When a member of the household is diagnosed with celiac disease, it can be difficult to prepare a separate gluten-free meal.
In these cases, it may be more practical, at the discretion of the household, to switch to a fully gluten-free diet for the entire family. Finding a support group is also a great way to share your experiences and hear the experiences of others.
How Can One Be Aware of the Hidden Gluten in Packaged Products?
Patients should be educated to read labels on all prepared foods and condiments.
Patients having a meal at a restaurant should clearly and strictly notify the server that they must have their food prepared separately from any gluten-containing products. Alcoholic beverages such as beers, ales, and lagers should be avoided unless they are clearly labeled as gluten-free.
While milk does not contain gluten, it should be avoided initially due to secondary lactose intolerance. (5)
How Long Does It Take for the Intestines to Heal From a Flare-Up?

If strictly followed, a gluten-free diet should result in significant improvement in nearly three-fourths of patients within the first month.
Laboratory evaluation can be considered 4–6 weeks after adherence to a strict gluten-free diet to assess for improvement in anemia, vitamin levels, and serologic levels. (6)
Repeat upper endoscopy with biopsy can be considered 6 months after initiation of a gluten-free diet to confirm an appropriate response.
Final Word
Gluten is everywhere, which is why it can be difficult to avoid. Fortunately, a range of products available labeled as gluten-free are available. People with celiac disease have to be on their guard when buying or ordering food since even the slightest trace of gluten can aggravate their digestive symptoms.
Thus, you must always check the labels of your food products and inquire about the ingredients from the restaurant staff when dining out. The rule is to assume that every food item has gluten in it unless proven otherwise.
Living with such a food sensitivity can be a great inconvenience, but it can be managed through proper dietary regulation and lifestyle changes. As you grow accustomed to the routine, the problem will become less of a nuisance.
- Was this article helpful?
- YES, THANKS!NOT REALLY


