In this article:
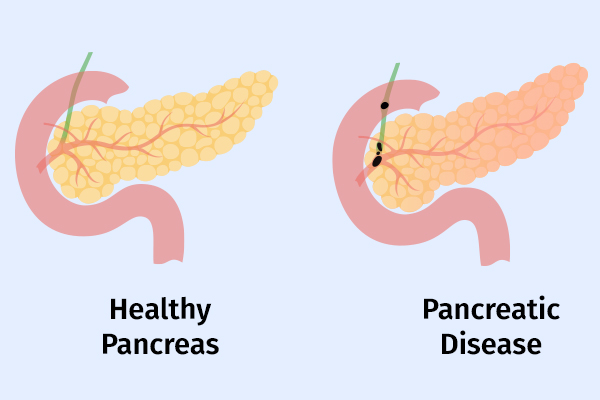
Acute pancreatitis is an irritation of the pancreas that can lead to serious inflammation throughout the body. It is very common and is most often caused by gallstones or alcohol use. (1)

Most cases of acute pancreatitis are mild (80%). However, severe pancreatitis is associated with high mortality rates. Acute pancreatitis typically presents with sharp abdominal pain that may travel to the back and is associated with nausea. It usually requires hospitalization.
The diagnosis is established with two out of the three criteria present, namely, typical symptoms, abnormal blood work, and abnormal CT scan. The treatment for acute pancreatitis is aggressive intravenous fluid resuscitation, bowel rest, and pain control.
Common Causes of Acute Pancreatitis
The cause of pancreatitis is most commonly due to alcohol use or gallstones.
Less common causes of acute pancreatitis include:
- Hypertriglyceridemia
- Medications
- Trauma
- Hypercalcemia
- Genetic disorders
- Vascular disorders
- Infections
- Having undergone ERCP (endoscopic retrograde cholangiopancreatography)
However, in up to 40% of patients, the cause is never elucidated.
Symptoms of Acute Pancreatitis
Typical symptoms of acute pancreatitis include sharp abdominal pain that pierces through the back. Other symptoms of acute pancreatitis include:
Medical Treatment for Acute Pancreatitis
Doctors will attempt to find the reason for the attack of acute pancreatitis.
- If the reason is alcohol use, then counseling regarding alcohol abstinence will be provided before leaving the hospital.
- If it is determined that the attack was due to gallstones, then a consultation with a general surgeon will ensue for an early cholecystectomy (removal of the gallbladder), preferably before leaving the hospital. (2)
- In older individuals without identification of a specific cause for the attack, an outpatient follow-up with a gastroenterologist within a few weeks of leaving the hospital is imperative. Acute pancreatitis can be the earliest clinical presentation of pancreatic cancer, and thus a close follow-up is prudent.
- A small group of patients with acute pancreatitis may require an endoscopic procedure during hospitalization. This type of endoscopy is called an endoscopic retrograde cholangiopancreatography (ERCP). (1)
Duration of Acute Pancreatitis
Generally, symptoms of mild, uncomplicated forms of acute pancreatitis resolve within a couple days to a week.
However, in acute pancreatitis associated with complications, the course is prolonged and can last weeks to months. Recurrence of complications is also common, thus necessitating a return to the hospital for re-evaluation.
Lifestyle Changes for People With Acute Pancreatitis

These healthy lifestyle changes can help speed up recovery from acute pancreatitis:
- Give up alcohol, cigarettes, and tobacco.
- Consume a low-fat diet to minimize the risk of gallstones.
- Drink plenty of water.
- Keep your body weight within the healthy range.
Dietary Precautions for People With Acute Pancreatitis
There are no foods that necessarily “cause” pancreatitis.
Once diagnosed, however, any intake by mouth will aggravate the pancreas and cause more pain as well as inflammation. Therefore, upon initial diagnosis, all intake by mouth is withheld and fluid losses from the inflammation are replaced through intravenous resuscitation.
Once the pain improves (usually after 24–48 hours in mild cases), a diet is resumed. Current recommendations state immediate initiation of low-fat solid food rather than gradual introduction with advancements of the diet is best. (3)
Efficacy of Supplements for Relieving Acute Pancreatitis
No supplements are recommended to treat the pain associated with acute pancreatitis. Pancreatic enzyme supplements do not relieve abdominal pain and are prescribed only for patients with chronic pancreatitis and specifically pancreatic insufficiency. (4)
Drug-Induced Pancreatitis
There are no safe natural remedies for the treatment of acute pancreatitis. There are, however, medications and supplements that have been associated with the development of acute pancreatitis.
Drug-induced pancreatitis is not a common cause of pancreatitis (0.1%–2% of cases) but can lead to very severe cases. These medications can be looked up in an online database where they are usually categorized as class Ia, Ib, Ic, II, III, or IV based on the likelihood of this medication being the culprit for the attack. (5)
Class Ia drugs will have at least one case report in the literature in humans with a positive rechallenge in the setting where all other causes, such as alcohol, gallstones, hypertriglyceridemia, and other drugs, have been ruled out.
Examples of class Ia medications include mesalamine, acetaminophen, and erythromycin.
Strict Prohibition of Alcohol and Tobacco for People With Acute Pancreatitis

Alcohol and tobacco should be avoided after an episode of acute pancreatitis. Acute pancreatitis is the beginning of a continuum of pancreas diseases such as chronic pancreatitis and pancreatic cancer.
Individuals who have had pancreatitis are more likely to develop a “fatty pancreas” as a metabolic sequela due to intrapancreatic fat deposition.
Alcohol and tobacco use further contribute to the fatty deposition in the pancreas, which in turn may lead to progression to chronic pancreatitis or recurrence of acute pancreatitis. (6)
The Fatal Nature of Severe Acute Pancreatitis
Most cases of acute pancreatitis tend to be mild, but it can take a serious turn in up to 20% of the patients.
Mortality is directly associated with the number of organs that have failed as a result of the inflammatory response, the duration of organ failure, (7) and the timing of the organ failure (within the first week associated with higher mortality).
In severe pancreatitis, portions of the gland may die and become infected, which is referred to as infected pancreatic necrosis. Pancreatic necrosis due to multidrug-resistant organisms also increases the mortality risk. With severe forms of pancreatitis and multiorgan failure, mortality is as high as 45%. (8)
Effects of Acute Pancreatitis on Bowel Movement

Acute pancreatitis can lead to reduced bowel movements and retention of abdominal gas. The inflammation in the pancreas can affect nearby structures such as the small bowel (9) and colon.
Given that the treatment of acute pancreatitis is bowel rest, the lack of eating also contributes to reduced bowel movements during the attack. In most cases, bowel movements return to normal once the inflammation subsides.
Personal Insights About Treating Patients Acute Pancreatitis
I had the pleasure of treating a 57-year-old gentleman who presented to the hospital with a second episode of acute pancreatitis. He was complaining of severe pain, nausea, and inability to tolerate food.
A CT scan noted a 4-cm cyst by his pancreas, likely a complication of his prior attack. There was also a lot of inflammation surrounding the beginning segment of his small intestine.
We performed an endoscopic procedure and drained his cyst. However, he continued to complain of pain with food intake and thus was still unable to eat.
We performed an innovative procedure by placing a temporary stent from his stomach to the small intestine, bypassing the area of the intestine directly abutting his pancreas that appeared inflamed on the CT scan.
After the procedure, he began to tolerate liquids. We advanced him to solid food, and shortly thereafter he left the hospital. Upon evaluation in the clinic one month later, he was feeling well and had put on weight. We scheduled him for a repeat endoscopy to remove the stent, which he tolerated without any issues.
Final Word
Complications of acute pancreatitis can arise within a few days or weeks of the initial attack or after 4 weeks.
A follow-up with a gastroenterologist after leaving the hospital is important if you experience recurrent abdominal pain, nausea, vomiting, trouble eating, losing weight, fevers, or significant changes with your bowel movements (such as diarrhea).
- Was this article helpful?
- YES, THANKS!NOT REALLY


