In this article:
The tonsils are embedded in the upper respiratory tract and a component of the immune system. Their main function is to screen the pathogens that come through the mouth with its large surface and antigen-presenting cells and to rapidly activate the immune system to take care of pathogens, leading to the release of macrophages, T lymphocytes, and B lymphocytes.

The tonsils are part of the development of the immune system, and they should continue to grow in children until 6 years of age. Then, their size begins to decrease until it stabilizes by the age of 12.
Children under the age of 6 are prone to tonsil infections and inflammation (tonsillitis) (1) because they have immature immune systems, they are consistently exposed to airborne infectious pathogens due to close contact, and they have rapid tonsil expansion.
In individuals 15 or older, tonsillitis is less common given the stabilized tonsils size and more robust immune systems.
Tonsillitis in Children and Its Types
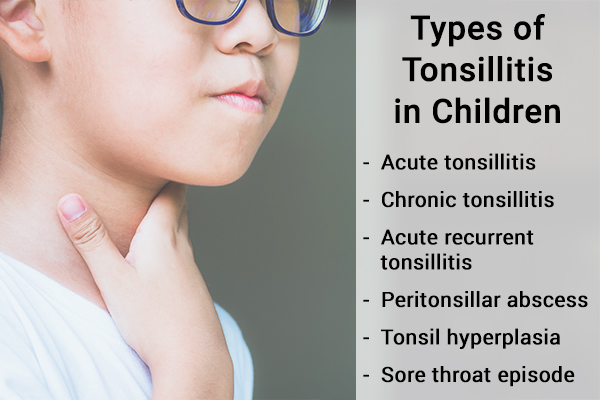
In a nutshell, tonsillitis is simply an infection of the tonsils in a child due to a variety of infections, including viral, bacterial, and fungal. (2)
Regardless of the etiology, tonsillitis is subclassified into the following based on the clinical presentation and complications:
- Acute tonsillitis: This is the typical tonsillitis most individuals recognize with a fast onset of symptoms of fever and sore throat. It is commonly caused by bacterial or viral infections. Acute tonsillitis is commonly accompanied by an upper respiratory infection.
- Chronic tonsillitis: This is a prolonged tonsil inflammation despite treatment. The definition of duration of treatment varies slightly from one medical specialty to another, but the common consensus is 4 weeks of treatment without real improvement. Infections are most likely the cause of chronic tonsillitis, but since the symptoms persist despite treatment, further workup is needed to evaluate for other causes such as an underlying inflammatory process or malignancy.
- Acute recurrent tonsillitis: This type of tonsillitis presents very similarly to acute tonsillitis but tends to recur and flare up a few weeks after treatment. The cause is still more commonly infections. However, if the clinical presentation fits the symptoms of PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis) and other inflammatory diseases, illness must be considered.
- Peritonsillar abscess: This is one of the more serious complications of tonsillitis where there is abscess(es) in or around the tonsils. Depending on the size and location, this type of tonsillitis can be considered a medical emergency due to its ability to obstruct airflow in a child. Peritonsillar abscess is commonly caused by bacterial infection; viruses tend to play little or no role in it.
- Tonsil hyperplasia: This type of tonsillitis refers to tonsil enlargement without a clear cause. Many of the children affected by this condition are not in distress. It is common for doctors to discover on further examination an enlarged tonsil at stages 3–4. (3) The cause of enlarged tonsils can vary, and they can cause partial airway obstruction in a child. If a child complains of constant fatigue with unrestful night sleep, obstructive sleep apnea secondary to enlarged tonsils must be evaluated.
- Sore throat episode: This is when the diagnosis of tonsillitis is unclear. The child has the clinical presentation, but there are no clear-cut examination findings to differentiate throat infection/inflammation (pharyngitis) from tonsillitis.
Causes of Tonsillitis in Children
Infections of the tonsils are likely just infections of any body part caused by various pathogens, from viruses and bacteria to fungi: (4)
- Viral: Epstein-Barr virus, cytomegalovirus, adenovirus, enterovirus (coxsackie A and B), herpes, human immunodeficiency virus (HIV), influenza virus, respiratory syncytial virus (RSV), parainfluenza virus, rhinovirus, coronavirus
- Bacterial: Group A streptococcus, Mycoplasma pneumoniae, Corynebacterium diphtheriae, Neisseria gonorrhoeae, Arcanobacterium haemolyticum, other streptococci (groups G and C), Haemophilus influenzae type b, Francisella tularensis, Fusobacterium necrophorum, Chlamydia pneumoniae, Chlamydia trachomatis, Yersinia enterocolitica, Coxiella burnetii
- Fungus: Candida species
Signs and Symptoms of Tonsillitis in Children

Common signs and symptoms of tonsillitis are fever, throat pain, exudate on a child’s tonsils, and other nonspecific symptoms. Other associated symptoms such as specific types of rash can help identify the cause (group A streptococcus). Generalized, nonspecific symptoms involving multiple systems with cough, diarrhea, and others suggest viruses are more likely the cause.
Most of the uncomplicated tonsillitis cases can be treated with antibiotics and supportive care. Some of the associated symptoms such as stridor at rest, neck stiffness, limited neck movement, drooling, tripod sitting position, abnormal neurological findings, respiratory distress, or toxic appearance may suggest more concerning underlying causes.
The most alarming complications/causes include by not limited to epiglottis (mostly on unimmunized children), severe peritonsillar abscess, retropharyngeal abscess, or Lemierre’s syndrome (infectious blood clot to internal jugular vein). (4)
If any of these concerning findings are present, the child must be evaluated by a medical professional promptly for immediate treatment.
Treatment of Tonsillitis in Children
The treatment plan for tonsillitis is largely dependent on the underlying cause.
Bacterial tonsillitis
Antibiotics such as penicillin or amoxicillin are very effective against the many bacterial causes of tonsillitis. Macrolide antibiotics such as Z-pack are very effective against atypical bacteria.
Regardless of the etiology, part of the treatment is pain control and ensuring hydration. For pain control, NSAIDs such as ibuprofen can help reduce systemic pain. (4)
Hydration is paramount
In addition to pharmacological treatment, hydration is also paramount with any illness. With tonsillitis, children often have throat and oral pain, which makes fluid intake a challenge.
In my practice, I found that, with ill children, nondairy-based ice popsicles can be a great way to rehydrate the child. The coolness of ice popsicles tends to numb the oral pain while each ice popsicle contains 1–2 ounces of fluid for rehydration.
Chronic or recurrent tonsillitis
For chronic or recurrent tonsillitis, treatment also varies depending on the cause.
- If the child has recurrent group A streptococcus infection, an additional treatment of clindamycin may be provided to eradicate the child’s possible carrier status.
- Otherwise, the ultimate treatment for the tonsillitis is the removal of tonsils (tonsillectomy).
Tonsillectomy was more commonly performed by otolaryngologists in the past due to its effectiveness against tonsillitis. Recently, more studies suggested that the procedure might not be as effective as it was thought to be, and there are long-term respiratory and immunological complications. (5)
Given the newfound concern with chronic complications associated with tonsillectomy, otolaryngology-head and neck surgery came up with a stricter practice guideline on tonsillectomy.
For a child to be considered as a tonsillectomy candidate, a child must have:
- Recurrent throat infection greater than seven times per year, five times per year for 2 years, or three times per year for 3 years (6)
- Otherwise, the child must have some more severe type of tonsillitis such as more than one episode of peritonsillar abscess or underlying inflammatory condition, such as PFAPA.
Diagnosing Tonsillitis in Children
The diagnosis of tonsillitis is mostly based on the clinical history and results of the physical examination. Laboratory studies such as viral/bacterial antigens or PCR studies can help physicians identify the cause of tonsillitis (4) so appropriate treatment can be given.
In more severe forms of tonsillitis such as peritonsillar abscess and retropharyngeal abscess, head and neck radiograph such as a simple x-ray or computer tomography is necessary to evaluate the extent of the lesion.
Preventing Tonsillitis in Children
Since tonsillitis is mostly infectious in origin, infection control is the best way to prevent the illness. Here’s how to do it:
- First, ensure that the child’s vaccination is up to date. Although childhood vaccination does not cover all causes of tonsillitis, it does cover pathogens such as H. influenzae and C. diphtheriae, reducing the child’s chance of getting a more severe disease.
- Second, the child must be taught to practice good basic infectious control by following the 3 Ws (wash your hand, wear a mask, and watchful distancing). The second prevention strategy is lessons learned from COVID transmission studies in North Carolina school districts. By simply mandating the 3 Ws during the COVID pandemic, the school districts can remain open, and the school transmission rate is essentially zero. By extension, if children can be taught to make the effort to apply the 3 Ws at any public setting, any infections transmission can be significantly reduced.
General Queries
Is tonsillitis contagious?
Yes, tonsillitis is contagious due to the various infections causing it. The level of contagiousness depends on the pathogens. Viral causes such as adenoviruses and flu viruses can be airborne, while bacterial causes such as streptococcus require close contact or droplets.
Can tonsillitis in children go away on its own?
Yes, most tonsillitis goes away on its own when the infection is properly treated or resolves on its own. If a child has recurrent or chronic tonsillitis, further study must be performed to rule out underlying chronic illness.
How long does tonsillitis normally last?
The typical acute tonsillitis can last for 7–14 days depending on the infectious pathogens. In the case of recurrent or chronic tonsillitis, a child must receive additional workout to rule out other chronic causes of tonsillitis.
Final Word
Tonsillitis is usually self-resolving but can be quite discomforting while it lasts. Plus, extra care must be taken not to pass the infection to others, and stringent hygiene is the best way to ensure that. Since children are not very mindful of these precautions, parents have to be on guard.
Tonsillitis is rarely a health scare, but prompt medical attention is needed if the child develops breathing problems, especially during sleep. Sudden onset of snoring is a sign of respiratory distress and should be taken seriously.
- Was this article helpful?
- YES, THANKS!NOT REALLY


