In this article:
Neonatal jaundice, also known as neonatal hyperbilirubinemia, is a form of jaundice that affects infants in the initial few days or weeks of their life.

The overwhelming prevalence of this condition can be gauged from the fact that about 60% of the babies born after a full-term pregnancy suffer from it, while 80% of all premature newborns are diagnosed with it.
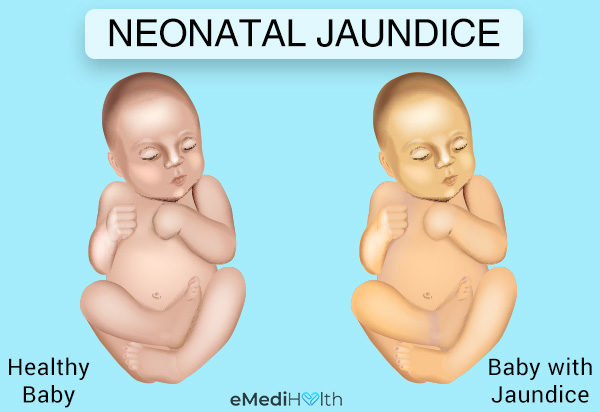
At the onset of this type of jaundice, your baby’s facial skin and whites of the eyes acquire a yellowish hue, which then spreads further down to the chest and abdomen. In some cases, the discoloration may reach as far as the umbilicus. In rare cases, it may reach the lower extremities to encompass the whole body.
In addition to the skin, jaundice can also stain your baby’s eyes and mouth. This first visible sign of neonatal jaundice usually appears 2–4 days after the child is born, and the condition can last for as long as 1–2 weeks.
Types of Jaundice
A newborn can develop jaundice due to several reasons.
a. Physiologic vs. pathologic jaundice
1. Physiologic jaundice
Most cases of neonatal jaundice are physiological in nature. A baby’s liver is often too immature to function adequately and has a relatively limited capacity to remove the bilirubin from the bloodstream or excrete it through the stool.
It is due to this suboptimal liver function that babies are particularly prone to developing an excess of bilirubin in their body soon after they are born.
2. Pathologic neonatal jaundice
Pathologic jaundice is relatively more serious and long-lasting than normal physiologic jaundice. This form of neonatal jaundice is the result of an underlying health problem that further compromises your baby’s already underdeveloped liver function and adds to the bilirubin load.
The following conditions can either increase the production of bilirubin or hamper its clearance and are recognized as the most common culprits for the onset of pathological jaundice in neonates:
- Hypothyroidism
- Rhesus factor disease
- Immune or nonimmune hemolytic anemia
- Inherited conditions such as Crigler-Najjar syndrome and glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Structural defects in the bile ducts and gallbladder.
For this kind of jaundice to resolve, it is essential to identify and treat the underlying condition that is responsible for the bilirubin buildup.
To that end, the doctor will focus his efforts towards diagnosing the pathologic cause of the jaundice and then suggest the appropriate treatment for it. The aim of treatment is to address the root cause of the problem in a timely manner.
b. Breastfeeding jaundice
Infants who are fed with their mother’s milk have a greater tendency to develop a moderate form of physiologic jaundice in their early days, as opposed to those who are given formula or are bottle-fed. Because they are still adjusting to the process of suckling, breastfed newborns tend to have a largely erratic feeding pattern, which can deprive them of the calories and hydration they need.
Additionally, the mother may not be producing enough milk to meet the baby’s requirement, which can also contribute to this kind of early-onset neonatal jaundice. Breastfeeding jaundice occurs in almost one-sixth of all breastfed infants, typically during the first week after birth.
c. Breast milk jaundice
Breastfed infants may also develop increased levels of bilirubin in the body during the second or third week of life or even later, resulting in a different kind of delayed neonatal jaundice.
Although the reasons for this late-onset breastmilk jaundice are not clearly understood, it may have something to do with the composition of the breastmilk.
Maternal milk contains certain substances that can make it difficult for the liver to metabolize bilirubin and remove it from the blood. Instead, the waste product is reabsorbed by the intestine, resulting in its persistently high levels in the blood. In most cases of breastfeeding jaundice and breastmilk jaundice, doctors recommend that the mother continues breastfeeding.
Causes of Neonatal Jaundice
The discoloration observed in neonatal jaundice is due to the buildup of a yellowish bile pigment called bilirubin in the blood. High levels of bilirubin in the body manifest as unusually yellow-looking skin.
Bilirubin is essentially a naturally occurring waste product that forms when your body breaks down old and damaged red blood cells to make new ones.
A newborn has to undergo rapid physiological changes soon after birth to get accustomed to the new environment. Switching from life in the womb to the actual world calls for the replacement of used red blood cells with a fresh supply of blood.
Red blood cells contain an oxygen-carrying protein called hemoglobin, which is converted to bilirubin inside the liver during the breakdown of the old, used cells. In a healthy, well-functioning body, the liver filters out bilirubin from the blood and flushes it out of your system.
As newborns do not have a fully developed body mechanism, their liver may not function fast enough to eliminate this waste product, resulting in jaundice. In addition, a major way the body eliminates bilirubin is through the stool, and newborns may not yet be having enough bowel movements to excrete the bilirubin.
Signs and Symptoms
Most cases of neonatal jaundice show their first sign around 2-4 days after birth and tend to resolve within a matter of 2 weeks.
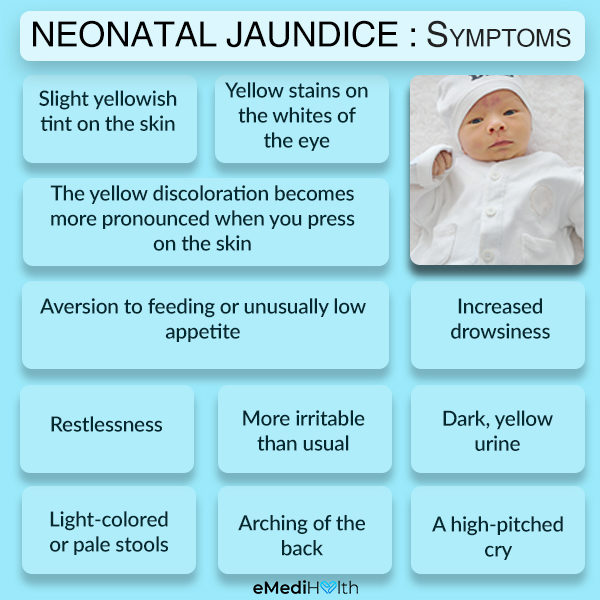
Babies with an excess of bilirubin in their body may display the following common symptoms which usually resolve with feeding and time:
- Slight yellowish tint on the skin
- Yellow stains on the whites of the eye
- Yellow discoloration that is more pronounced when you press on the skin
The above-listed symptoms are fairly non-threatening and do not require medical assistance. However, you must call your pediatrician in case you notice more concerning symptoms like the following:
- Aversion to feeding or unusually low appetite
- Increased drowsiness
- Restlessness
- More irritability than usual
- Dark, yellow urine
- Light-colored or pale stools
- Arching of the back.
- A high-pitched cry
A high bilirubin level can jeopardize your baby’s health in more ways than one and warrants proactive medical care. The bilirubin test results are assessed along with the baby’s age and other risk factors to determine what treatment and follow up are needed.
Medical Treatment
The treatment for neonatal jaundice depends upon its severity.
a. Mild cases
Mild neonatal jaundice in an otherwise healthy infant usually resolves without any medical intervention. The extra bilirubin is processed by the liver and cleared from the body in a few days.
b. Moderate cases
1. Phototherapy
The routine treatment for moderate neonatal jaundice is phototherapy. This treatment method involves shining a special type of blue fluorescent light on the baby’s bare skin or laying the baby under a phototherapy light blanket to maximize the exposure of skin to the lights.
The blanket may also be used to cover the baby while the mother holds the baby skin to skin while bonding or breastfeeding.
Exposure to this light leads to the breakdown of bilirubin into a simpler form through a process called photo-oxidation. Photo-oxidation of bilirubin means that the waste substance acquires extra oxygen to become more soluble in water. This makes it easier for the baby’s immature liver to process the simplified form of bilirubin and flush it out of the body along with the urine or stool. (1)
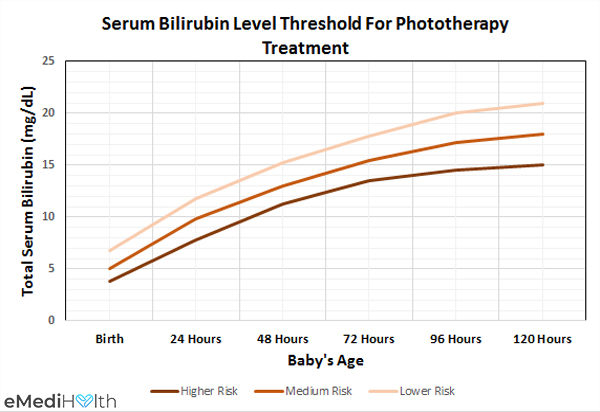
Elevated TSB levels can prove more dangerous for some babies than others, which largely depends on their gestational age and whether they have any associated risk factors. The above-given chart demonstrates the differential risk of increased bilirubin in neonates.
Lowest risk: Babies with a gestational age of 38 weeks or more who are otherwise healthy and devoid of any associated risk factors are least susceptible to neonatal jaundice.
Medium risk: Babies with a gestational age of 38 weeks or more who happen to have certain associated risk factors as well are at medium risk of developing neonatal jaundice.
Highest risk: Babies with a gestational age of less than 38 weeks (between 35-37 weeks) and some associated risks factors as well are most likely to develop neonatal jaundice.
Phototherapy is broadly divided into:
- Conventional phototherapy: The jaundiced baby is stripped down to his diaper and placed under a halogen or fluorescent lamp with his eyes covered by a protective gear. The jaundiced baby is laid in a warm incubator under blue fluorescent lights, wearing only his diaper and eye protection.
- Fiber-optic phototherapy: The doctor may place the jaundiced infant on a blanket woven with fiber-optic cables with light streaming through it to expose his back to phototherapy. The doctor may wrap the baby in a biliblanket, which is a portable pad with fiber-optic fibers running through it. Placing the baby in this device exposes his skin to direct light.
Babies that are undergoing phototherapy for neonatal jaundice may experience the following:
- Prolonged exposure to lights can render your baby increasingly dehydrated, which may call for the intravenous administration of fluids during treatment.
- Your baby may have frequent and loose bowel movements with greenish-colored stools during the course of the treatment, which is their body’s way of eliminating the excess bilirubin from the body. If this condition persists even after the cessation of phototherapy, contact your baby’s pediatrician for assistance.
- The doctor will monitor the baby’s bilirubin level through blood tests and discontinue the phototherapy once the bilirubin load has been brought down to a safe degree.
2. Intravenous fluids
Neonatal jaundice is more common in breastfed infants, who may need intravenous fluids if their bilirubin level rises to a severe degree.
Breastfed newborns may find it difficult to meet their hydration needs through their mother’s milk as they struggle with suckling during the early days of their life or in some cases the mothers do not produce enough breast milk to meet their baby’s needs.
Maternal milk is also high in sodium, which also contributes to dehydration in breastfed infants. (2)(3)
c. Severe cases
- Neonatal jaundice in infants with blood type incompatibilities may be given intravenous immunoglobulin (IVIg) to block the maternal antibodies from attacking their red blood cells. This intervention may help reduce the baby’s dependence on exchange transfusions.
- Exchange blood transfusion involves replacing the baby’s blood with that of a healthy donor. Doctors usually resort to this complex procedure in emergency situations when phototherapy fails to deliver the desired results. This treatment strategy is used when the bilirubin levels become dangerously high and a rapid decline is needed.
Diagnosing Neonatal Jaundice
Diagnosing a case of neonatal jaundice begins with checking your baby’s bilirubin levels, usually through a blood test. There are some doctors who prefer to conduct a preliminary light meter test before getting the blood sampling done. This involves placing a light meter on the baby’s head, which will reveal a transcutaneous bilirubin (TcB) level. (1)
If this preliminary examination points towards an excess of bilirubin, the doctor will most likely order a blood test to get a more accurate reading of the total serum bilirubin (TSB) level.
The doctor will take into account the test results, the baby’s age in terms of hours, and other risk factors to come up with an appropriate treatment plan.
Tips for Parents and Caretakers
- It is essential to examine your baby on a daily basis for any obvious sign of jaundice. The yellowing of the skin is most visible in bright, natural light. If the discoloration is extremely faint, you can conduct a blanching test by gently pressing on your baby’s chest skin with a finger to see if it turns yellow.
- The yellowish tint is less apparent in dark-colored skin, in which case you should check your baby’s eye and inner mouth for signs of staining. The discoloration is also more obvious on the soles and the palms as the skin on these sites are comparatively thinner. The further down on the body the yellow color is visible, the higher the bilirubin level is. Thus, the yellow color in the eyes or mouth is less worrying than the staining of the lower abdomen or legs. This can be more difficult to access in babies with darker skin pigments, so the laboratory levels help to correlate findings. Parents should discuss this with their physician to help them understand how the current level looks in their baby.
- Keep your pediatrician updated about any changes in your baby’s condition, whether good or bad. If the yellowing of your baby’s skin becomes more pronounced than before, call your pediatrician immediately.
- Early-onset neonatal jaundice can lead to deleterious consequences for your baby’s health if not handled properly. A newborn requires prompt medical attention if this condition develops in the first 23 hours of life. It is an emergency situation and delayed treatment can put your baby in a critical condition.
- Make sure that your baby is well-fed to keep jaundice from worsening. Even if you suspect that breastfeeding may have caused jaundice, you must continue feeding the infant in accordance with the doctor’s guidelines. A newborn’s body requires a sufficient dose of nutrition and hydration to fight itself back to health in the case of neonatal jaundice. Babies need to have enough food and fluids in their system for their liver to process the excess bilirubin. Babies who derive their sustenance from maternal milk should be fed at least 8 to 12 times in a day, whereas bottle-fed infants should be given at least 6 to 10 feedings in a day.
- Exposing your newborn to direct sunlight for prolonged periods is not considered a safe treatment strategy for neonatal jaundice. Clinically administered phototherapy under the supervision of a specialist may prove far more effective in addressing neonatal jaundice with no adverse side effects. (4)
- It is essential to follow up with your pediatrician even after starting the treatment to make sure that your baby is making the desired progress. The doctor may conduct repeat blood samples to ascertain if the prescribed treatment is working or not.
Risk Factors
The following factors can make your baby increasingly susceptible to neonatal jaundice:
1. Premature delivery
Babies who are born before 35 weeks of gestation often have an underdeveloped liver, which makes them more vulnerable to neonatal jaundice.
Even relatively lower levels of excess bilirubin, which are considered non-threatening for full-term babies, can lead to jaundice in premature ones because their underdeveloped liver is less capable of processing bilirubin.
2. Incompatible blood type between the mother and the baby
Babies who do not share the same blood group or Rh factor with their mother have a greater likelihood of developing a rare form of neonatal jaundice.
When the different blood groups blend during the gestation period or at birth, the mother’s blood contains certain antibodies that target the baby’s red blood cells.
3. Bruising
A baby born with bruises on the body (due to birth injuries such as cephalohematoma or caput succedaneum on the scalp) is more likely to develop neonatal jaundice later.
A bruise is essentially a blotch of blackish-blue discoloration that appears on the skin when an underlying blood vessel is ruptured and spills blood. When the body repairs the damage to heal the bruising, there is a spike in the levels of bilirubin.
4. Others
Other conditions that can put your baby at an increased risk of neonatal jaundice include:
- Internal bleeding (hemorrhage)
- Bacterial and viral infections
Complications Related to Jaundice
Neonatal jaundice can escalate to a very severe degree if left untreated and pave the way for extremely dangerous health complications.
Jaundice is brought on by a buildup of bilirubin in the body, which is a toxic waste product that can cause lasting damage to the central nervous system if it reaches the brain.
Acute bilirubin encephalopathy (ABE) refers to an extreme state of hyperbilirubinemia, when there is so much bilirubin in the body that it spills into the brain and starts destroying the brain cells.
The toxic injury incurred by the nuclear region of the brain (also referred to as the kern) on account of ABE is called kernicterus. Babies with this condition are often permanently affected by neurodevelopmental problems. This kind of brain damage is quite rare and entirely preventable.
Early treatment for neonatal jaundice is a must to keep bilirubin levels in check. This is the only way to prevent the onset of acute bilirubin encephalopathy and kernicterus.
Babies who were born prematurely or those who are severely jaundiced require special attention as they are more prone to such complications. (5)
When to See a Doctor
It is important to seek urgent medical help if your jaundiced baby shows the following symptoms:
- If your baby is too tired to feed well.
- If your baby looks or acts sick.
- If the urine becomes dark or there are fewer than 3 wet diapers per 24 hours at 3 days of age and 5–6 wet diapers per 24 hours after 4 days of age.
- If the bowel movement is white. Black, green, and yellow are normal stool colors in newborns.
- If the yellow color can be seen below your baby’s umbilicus/belly button.
Moreover, you must get your baby to the doctor if he/she develops jaundice in the first 23 hours after birth or if the symptoms tend to worsen or become more prominent after a week.
Expert Answers (Q&A)
Answered by Dr. Brandi Lewis, MD (Pediatrician)
Jaundice is typically identified by a yellow color that appears in the skin and eyes, due to an increase in bilirubin level. Bilirubin is a normal component of every person’s blood.
However, when bilirubin rises above a certain level, it can become dangerous. Due to immature liver processes, most newborn babies develop bilirubin levels that are higher than adult levels.
Therefore, most babies develop some degree of jaundice. When bilirubin levels become too elevated, it becomes dangerous to the newborn.
In developed countries such as the United States, mortality from jaundice is not high. This low mortality is due to screening practices that take place in birthing hospitals and early interventions done by pediatricians within the first few days of life. (6)
Most babies do not experience complications from jaundice. However, newborns who develop very high levels of bilirubin are at risk for brain injury.
Some consequences of elevated bilirubin in newborns are reversible and some are not. Immediate consequences can be difficulty eating, problems breathing, fevers, and seizures. Long-term consequences can be cerebral palsy (CP) and problems with hearing and vision. (7)
Babies born with any of the following are at higher risk for complications due to jaundice:
• Jaundice that developed within the first 24 hours of life
• Infants who were considered high risk based on lab work done in the birth hospital
• Infants with inherited blood disorders (such as G6PD deficiency)
• Premature Infants (born earlier than 36 weeks gestation)
• Infants who had siblings that required treatment for jaundice
• Infants who are not doing well with exclusive breastfeeding and have high percentages of weight loss
• Infants with significant birth trauma
• Infants of East Asian race
For many infants, jaundice begins to improve after the fifth day of life, with resolution typically in the first 1-2 weeks after birth.
While sunlight is somewhat effective at improving jaundice, it is not recommended as a treatment.
Exposure to sunlight causes unnecessary risks such as sunburns, dehydration, and overheating. If a baby does require treatment, special blue lights are used that have been proven to be safe. (8)
Making sure your infant is feeding well is the most helpful remedy for jaundice. Bilirubin is removed from an infant’s body through urine and stool.
Therefore, the more they eat, the more urine and stool they make, and the quicker their jaundice resolves.
Here are some tips:
• Feed your infant frequently.
• Make sure they have an appropriate number of wet and dirty diapers.
• Monitor their stool changes. The stool color should change from dark brown to yellow.
After birth, all newborns should be examined and monitored to help prevent complications from jaundice. In the hospital, screening tests are done to evaluate their risk for high bilirubin levels.
Newborns should also be seen by their pediatrician within the first 3-5 days of life. Pediatricians are very good at identifying which babies need additional testing and which infants need treatment for their jaundice. (9)
- Was this article helpful?
- YES, THANKS!NOT REALLY



