In this article:
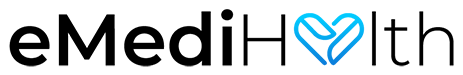
Juvenile rheumatoid arthritis (JRA), or juvenile idiopathic arthritis (JIA), is a chronic childhood illness that causes inflammation and pain in a child’s joint(s).

According to the International League of Associations for Rheumatology (ILAR), this chronic illness breaks down into seven different subtypes. It is categorized by the number of joint involvements, associated lab abnormality, and additional systemic features related to the illness.
To be diagnosed with JRA, the child must meet the following three criteria:
- Sixteen years old or under at the time of diagnosis
- Persistent synovitis (Inflammation of the joint space/fluid) for a minimum of 6 weeks
- All other diagnoses must be excluded. (1)
Prevalence of Juvenile Rheumatoid Arthritis
JIA affects about 300,000 children in the United States. The occurrences are 1–4 in about 10,000 annually in the United States, and its prevalence is about 1 in 1000 among the US pediatric population. (2)
Types of Juvenile Rheumatoid Arthritis
According to ILAR’s classification, there are currently seven subtypes of JRA:
- Systemic-onset JRA – Longer than 2 weeks of arthritis and fever, plus additional systemic symptoms such as red rash, lymph node enlargement, liver/spleen enlargement, or signs of joint fluid inflammation. This is equivalent to adult Still’s disease.
- Polyarticular RF negative – Arthritis in more than 5 joints within the first 6 months of disease with negative rheumatoid factor on blood draw.
- Polyarticular RF positive – Arthritis in more than 5 joints within first 6 months of disease with positive rheumatoid factor on blood draws that are 3 months apart. This is equivalent to adult rheumatoid arthritis (RF+).
- Oligoarthritis – Arthritis affecting less than 4 joints with 2 subtypes. First, the persistent subtype is affecting no more than 4 joints. Second, the extended subtype affects more than 4 joints after 6 months of disease.
- Enthesitis/spondylitis-related JRA – Signs and symptoms of joints, ligaments, and tendon inflammation. It is often accompanied by systemic and lab abnormalities. Patients usually complain of hip and back pain along with inflammation of the eye, and HLA-B27 is positive on lab draw. This arthritis tends to have a strong family history of other systemic inflammatory illnesses such as inflammatory bowel disease.
- Juvenile psoriatic arthritis – Arthritis accompanying psoriasis skin findings. It is also often associated with a strong family history and abnormal nail findings.
- Undifferentiated arthritis – Chronic arthritis that does not fully meet the criteria of a single individual category above. (3)
Triggers and Causes of Juvenile Rheumatoid Arthritis
The triggers and causes of JRA are unclear. While there are multiple competing hypotheses and proposed mechanisms of illness, all experts can agree the illness originated from the dysregulation of the immune system. The triggers being proposed so far are generally not easily avoidable, such as viral, environmental, and more induce immune dysregulation. (4)
Common Symptoms of Juvenile Rheumatoid Arthritis
Common signs and symptoms of JRA are as follows:
- Morning stiffness that improves with movement later in the morning
- Change in walking, running, climbing, and willingness to play
- Loss of ability to dress, feed, bathe, or toilet oneself
- Enuresis with a previously toilet-trained child
- Developmental regression
- Leg-length discrepancies
- Fever, liver/spleen enlargement, rash, gastrointestinal symptoms, and eye symptoms for the different subtypes (3)(4)
Treatment Plan for Juvenile Rheumatoid Arthritis

Unfortunately, there is no single cure for JRA. It is a very heterogeneous disease; therefore, its treatment plan often depends on its subtype and severity.
Ibuprofen can be used for symptom control for some of the very mild forms such as oligoarthritis. The more severe or more persistent form of JRA requires disease-modifying antirheumatic drugs (DMARDs) to better control the chronic illness.
Some of those older DMARDs can induce serious side effects as some of these agents have been used as immunosuppressants. For instance, cyclosporine is often used in mast cell activation syndrome in patients with systemic JRA, and methotrexate is used as a chemo agent to induce remission.
The newer DMARDs are known as a group of monoclonal antibodies, and their generic names commonly end with -mab. They tend to have less toxic side effects than the older generation.
Many of the new monoclonal antibodies are the preferred choice of treatment for pediatric rheumatologists and by treatment guidelines, but only a handful of them have full FDA approval for usage in pediatric patients.
The goal of therapy for all DMARDs is the same, which is to prevent flare-ups and reduce the need for systemic steroid usage in patients. (5)
Diagnosing Juvenile Rheumatoid Arthritis
To diagnose JRA, the doctor will generally follow these steps:
- Obtain a thorough and detailed history of a patient’s recent clinical course.
- Check the child’s detailed family history with a strong emphasis on rheumatological illness.
- Perform a detailed head-to-toe physical examination with extra attention to skin lesions and other signs and symptoms of systemic illness.
- Order laboratory studies with complete blood count, inflammatory markers, and rheumatological markers to further solidify the diagnosis.
Lifestyle Changes and Home Remedies for Juvenile Rheumatoid Arthritis
Alternative treatments for JRA are largely not proven currently. There are no reputable peer-reviewed papers that suggest the disease process can be improved with any alternative therapy or home remedy.
However, complementary therapy, which involves eating better and living healthier, may improve the patient’s immune system. In addition, daily exercise habits and mindfulness can help reduce anxiety and possibly help the child to manage the pain with fewer medications.
Lifestyle modifications are also known as complementary and alternative medical (CAM) therapies. In a small retrospective study, it was found that the use of certain CAM therapies made patients and their parents much more content with the overall treatment plan but had no real effect on the overall disease process. (6)
Complications Associated With Juvenile Rheumatoid Arthritis

In certain types of oligoarticular/polyarticular JRA, patients are at an increased risk of uveitis (eye involvement). They must follow up with an ophthalmologist on a yearly basis.
A patient with an enthesitis subtype is at an increased risk of other inflammatory illnesses such as inflammatory bowel disease. A follow-up with a gastroenterologist would be essential to improve the patient’s overall health.
Other than the long-term complications resulting from the chronic illness, systemic JRA has one of the most fearsome complications known as mast cell activation syndrome (MAS), which in some severe cases is a medical emergency.
MAS is a systemic activation of mast cells in the patient’s body that can cause anaphylactic-like symptoms such as constriction of the airway causing difficulty breathing, blood vessel dilation causing hypotension, and generalized pruritic rashes.
Patients experiencing an MAS attack need to be evaluated by a physician promptly. The treatment of choice varies, but many rheumatologists would use cyclosporine or sometimes monoclonal antibiotics to calm the patient’s immune system to prevent it from causing further inflammatory response to the body.
Most-Asked Questions About Juvenile Rheumatoid Arthritis
At what age does juvenile rheumatoid arthritis usually start?
Age of onset for JRA depends on its subtype but it is most commonly seen between 3 and 5 years of age. The common age of onset with each subtype is as follows:
- Systemic JRA – age 5–10
- Oligoarticular JRA – age 5
- Polyarticular JRA – age 1–3
- Psoriatic subtype – all ages
- Enthesitis-related subtype – more common in older children
Can juvenile rheumatoid arthritis come back in adulthood?
Yes, and it all depends on the subtype of JRA. While some subtypes are more likely to continue through adulthood, others tend to resolve on their own.
Is juvenile rheumatoid arthritis the same as rheumatoid arthritis?

Yes and no. Juvenile rheumatoid arthritis is an extremely broad heterogeneous disease. For some patients, the chronic symptoms can manifest themselves in adulthood. Sometimes, JRA can transform into rheumatoid arthritis once the child reaches adulthood.
Final Word
The specific treatment plan for juvenile rheumatoid arthritis is dependent on the subtype and severity, but the ultimate goal is always the same, which is to use the least amount of medications to keep the child from having an episode of acute flare-up.
Newer generations of DMARDs are becoming more favorable among rheumatologists and more widely used due to their efficacy and side effects profile, but the most common DMARD used to this day is still methotrexate. Sometimes, it is essential to start the patient with a systemic steroid such as prednisone to “cool down” the acute flare-up. (6)
- Was this article helpful?
- YES, THANKS!NOT REALLY