In this article:
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder that occurs when stomach contents frequently flow back up into the esophagus (food pipe).

Gastroesophageal reflux (GER) is a milder acid reflux condition and more common, especially in young children and infants. GERD is a more serious and a chronic condition and diagnosed by a physician.
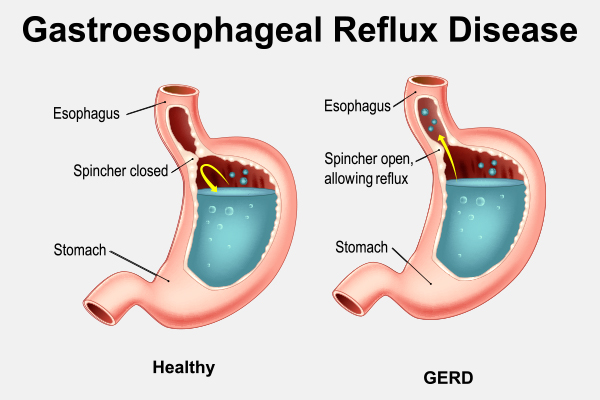
In people with GERD, the lower esophageal sphincter (the band of muscle at the lower end of the esophagus that usually prevents backflow of stomach contents) is abnormally relaxed or weakened, resulting in frequent acid reflux.
In children, GERD can lead to serious complications, including malnutrition and poor weight gain, if it is not diagnosed and treated. (1)
Treatment for GERD should be under the supervision of a pediatrician and usually includes medications and diet, lifestyle modifications. Diet plays a major role in managing the symptoms of GERD.
Pathophysiology of GERD in Children
The digestive process begins in the mouth, where food is chewed, mixed with saliva and swallowed. Swallowing pushes the food into the food pipe or esophagus to enter the stomach, where it undergoes further digestion.
The lower end of the esophagus that opens into the stomach is encircled by a muscular ring called the lower esophageal sphincter (LES). The LES remains tightly shut at all times and relaxes only to allow the ingested food or fluids to pass into the stomach. This closed valve prevents any backflow of stomach acids or contents into the food pipe.
However, a dysfunctional or weakened LES may open up when it’s not supposed to and allow the acidic gastric contents to flow back up into the esophagus, which is known as acid reflux.
This condition is common among children, especially infants and toddlers, because their digestive system is immature and still developing. Thus, they may not have fully formed or functional LES muscles, which can pave the way for acid reflux.
Children usually grow out of this phase as they become older. However, if acid reflux is frequent and becomes a chronic condition, it leads to GERD.
Common Symptoms of GERD in Children
Symptoms of GERD in children vary and may be different from those of adults with GERD. Common symptoms may be one or more of the following:
- Frequent regurgitation, spitting, or vomiting, usually after eating
- Gagging, choking, and hiccups
- Coughing often and having coughing fits at night
- Refusing to eat or eating only small amounts or being fussy around mealtimes
- Failure to gain weight
- Trouble swallowing
- Stomach pain
- A burning sensation in the chest or heartburn, usually after eating and which may be worse at night
- In children below 12 years, asthma symptoms including wheezing and dry cough
Foods That Are Good for Children With GERD

Diet plays a key role in the management of GERD in children. Nutrition therapy for GERD in children is generally focused on dietary modifications that aim to meet the child’s nutritional needs for optimal growth and development while also relieving the symptoms. (2)(3)
Integrated nutrition therapy, where parents or caregivers work closely with their child’s health care team members including the pediatrician and registered dietitian to implement individualized dietary modifications, is the most effective approach for long-term management of GERD.
Generally, healthy eating patterns emphasizing nutrient-dense foods including vegetables, non-citrus fruits, whole grain, and lean protein are recommended:
- Vegetables: A variety of nutrient-dense vegetables. Few examples are greens, celery, cucumbers, root vegetables (sweet potatoes, carrots, beets), and cauliflower
- Fruits: A variety of non-citrus fruits such as melons, banana, apples, and pears
- Whole grains: A variety of whole grains such as oatmeal, brown rice, whole grain bread and cereals
- Lean protein: Eggs, fish, and plant-based proteins such as lentils, beans
Foods That Can Worsen GERD in Children

Foods do not cause GERD, but some foods can aggravate the symptoms. The foods that worsen GERD are different for each child.
Parents or caregivers of children with GERD should maintain food diaries and record all foods consumed daily to identify and avoid foods triggering GERD symptoms.
In general, it is best to avoid or limit the following foods known to aggravate GERD symptoms: (4)(5)
- High-fat foods such as fried foods, fast food, pizza, processed snacks, potato chips, cheese, and meats high in fat such as bacon and sausage. These foods can be replaced with healthier food choices such as lean protein and plant-based foods and by baking instead of frying.
- Acidic foods and juices such as citrus fruits, tomatoes, and tomato-based sauces
- Spicy foods, chilies, onions
- Chocolate
- Peppermint
- Coffee, tea, and other caffeine-containing beverages
- Carbonated drinks
Lifestyle Changes for Managing GERD in Children
Timing of the meals is as important as the type of foods consumed for relieving symptoms of GERD: (6)
- Consume small, frequent meals instead of large, caloric-dense meals.
- Avoid eating just before lying down. Eat dinner at least 3 hours before going to bed.
- If the child is overweight or obese, weight management under the supervision of a health care provider is recommended.
Managing Acid Reflux in Bottle-Fed Infants
Acid reflux is common in infants during the first year of life and typically improves during toddler years. (7) However, if reflux occurs frequently and is severe, it can affect the weight gain and nutritional status of the baby.
- It is important to seek medical help from a pediatrician immediately if parents or caregivers notice any abnormal reflux symptoms.
- Generally, for bottle-fed babies with mild reflux symptoms, holding the baby in an upright position for 30 minutes after feeding and burping often during feeding are recommended.
- Overfeeding should be avoided.
- Pediatrician may recommend adding a small amount of rice cereal to the formula as thickener. This should be done only under medical supervision.
- In some cases where food intolerance or allergy is suspected in formula-fed infants, pediatrician may recommend a hypoallergenic formula.
- It is important to work closely with the pediatrician and health care providers to ensure optimum nutrition during this critical period of growth and development.
Can a Food Allergy in Children Cause Acid Reflux?
Food allergies and food intolerance are associated with acid reflux and worsened GERD symptoms. (8) Children can develop intolerance or allergic response to any food. However, dairy and wheat/gluten allergies are very common in children.
If food intolerance or allergy is suspected as the underlying cause of GERD symptoms, it is essential to seek medical care with the child’s pediatrician, who may recommend strictly eliminating the food causing the abnormal responses, which should be done under medical supervision.
If certain food or foods are strictly eliminated in the diet of children, it is essential to closely work with health care providers including registered dietitians to meet their nutritional needs and optimize their growth and development. (3)
For example, if a child develops a milk allergy, milk and milk-containing products must be avoided and safe alternative food choices need to be included to meet the nutritional needs, which should be done under the supervision of the health care providers.
Final Word
Diet and lifestyle play an important role in improving GERD symptoms. A healthy, balanced diet customized to meet the nutritional and lifestyle needs and food preferences of each child is important for long-term management of GERD.
Generally, healthy eating patterns that include nutrient-dense vegetables, non-citrus fruits, whole grains, and lean protein are recommended. Foods that are associated with GERD symptoms and generally trigger acid reflux should be avoided or limited.
Consuming smaller meals/snacks more frequently, avoiding large meals, and having dinner or a late-evening snack/beverage at least 3 hours before going to bed can help improve GERD symptoms.
Parents and caregivers of children with GERD should work closely with their health care providers including pediatrician and registered dietitian to ensure optimum nutrition to support their growth and development.
- Was this article helpful?
- YES, THANKS!NOT REALLY


