In this article:
Osteoarthritis (OA) is a degenerative disorder that targets every structural component of the joint. To say that OA causes wear and tear of the joints would be an overly simplistic representation of this condition, which involves:

- The progressive breakdown of the cartilage tissue that cushions the ends of your joint bones as well as the tendons and ligaments in the affected joint
- Bone deformity in the affected joint
- Inflammation of the synovium or joint lining
How Common Is It?
Arthritis is an umbrella term for more than 100 different types of joint disorders, both inflammatory and non-inflammatory.
OA is the most common form of arthritis, which usually affects people in the age group of 40 to 60. The joints most frequently affected include the hands, hips, and knees. (1)
The widespread prevalence of OA can be gauged from the figures released by the Centers for Disease Control and Prevention, which state that more than 32 million adults are diagnosed with this condition in the United States alone. (2)
Types of Osteoarthritis
OA is broadly classified into two types:
1. Primary OA
Most cases of OA fall in this category, whose defining characteristics are it is idiopathic and not set off by any condition.
While the cause behind this kind of joint degeneration remains unidentified, several factors can predispose you to this condition. Primary OA largely affects middle-aged and elderly populations.
2. Secondary OA
This kind of OA is relatively less common and usually has an early onset. Thus, it is more common in children and young adults.
Secondary OA gets its name from the fact that it typically stems from an underlying condition, such as infection, injury/trauma, prior surgery, underlying systemic disease (such as rheumatoid arthritis), underlying metabolic disorder, or congenital deformity. (3)
Causes of Osteoarthritis

OA occurs when there is a gradual breakdown of this smooth cushioning, which triggers increased friction between the articular surfaces whenever the joint is moved.
The wearing away of the cartilage exposes the frayed, rough surface of the underlying bone and makes joint motion increasingly painful.
Symptoms of Osteoarthritis
Although OA can manifest differently in different people, it is generally associated with the following symptoms:
- Stiffness and tenderness in the affected joint
- Joint pain, which typically is triggered or worsens with movement
- A crackling sound (crepitus) while moving
- Visible swelling of the joint
- Bony protrusions (osteophytes) around the affected joint
- Reduced function and mobility in the arthritic joint
- Decreased range of motion (flexion/extension) in the affected joint
- Muscle weakness around the affected joint, especially in the knee
- Joint deformity, which means that the affected joint eventually can become enlarged and/or malaligned
How Does Osteoarthritis Progress?
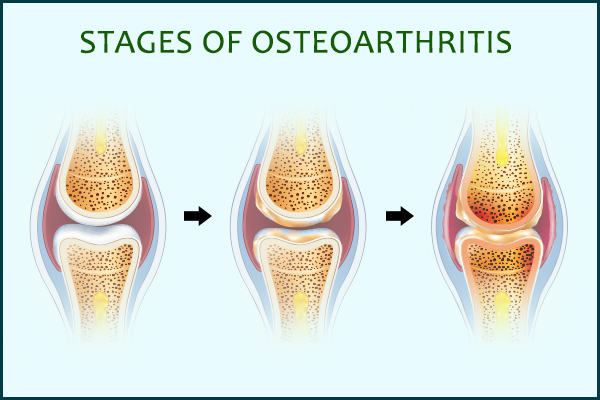
OA tends to worsen gradually, at times to a point where it becomes severely debilitating.
When the condition is in its initial stage, the patient will most likely experience the OA-induced pain during and after joint activity, but typically not otherwise. As the condition progresses to a more advanced stage, it can affect joint motion and use of the affected joint and limb.
When the condition becomes particularly serious, even the slightest activity can aggravate the joint pain, which may even be present while you are in a resting position. The pain can be accompanied by swelling and tenderness that can further hamper joint motion and function.
Types of Joints
The human body contains hundreds of joints that serve as essential links between different bones. Without joints, the entire skeletal system would be rendered immobile.
Joints can differ slightly in terms of their structure and material composition, but they are largely classified into three categories:
- Fibrous joints are completely immobile as they are filled with fibrous connective tissue with no space for movement.
- Cartilaginous joints are held together by a tough but flexible connective tissue called cartilage that allows little movement.
- Synovial joints contain a cavity between the connecting bones. The cavity is filled with a lubricating fluid that reduces friction between the adjoining bones and allows painless, unhindered joint movement.
The most movable joints are also the most prone to damage, which is why synovial joints are the worst affected by OA. The ends of the bones inside the joint are covered by protective padding of cartilage that allows them to glide easily against one another.
What Joints Are Most Affected by Osteoarthritis?
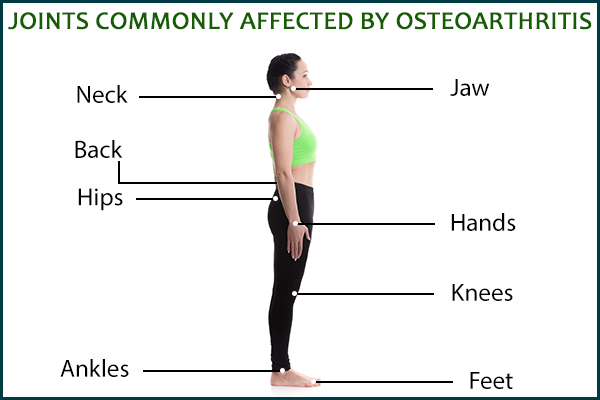
OA can damage any joint in the body, but the frequently used and weight-bearing ones are the most commonly affected.
1. Knees
Your knees carry the load of your entire body, making them especially prone to degeneration. Most people with OA experience pain and stiffness in their knees, which tend to get aggravated during or after a lower limb movement.
2. Hips
The large joints in the hips can develop OA, which is accompanied by radiating pain that can be felt not just in the buttocks but also in the front of the thigh, lower back, or groin area.
3. Lower back and neck
As a lot of possible causes can trigger back or neck pain, you need a proper diagnosis by a doctor to be sure.
4. Hands, feet, and ankles
OA can affect different joints in the foot, but most people experience symptoms at the base of the big toe and the middle section of the foot. The ankles tend to suffer the least damage.
Women are most affected by OA of the hands, usually when they are nearing the age of menopause.
5. Jaw
The constant jaw movement while talking, yawning, and eating can wear away the smooth cartilage in the temporomandibular joint, leading to the onset of jaw OA.
Risk Factors for Osteoarthritis
Some people are more prone to OA than others due to any of the following factors:
- Family history of OA
- Having OA in one body part: People who have hand OA are more likely to develop knee OA. (1)
- Being overweight or obese
- Severe or repeated trauma to a joint
- Prolonged overuse or misuse of a joint
- Joint infections: Several bacterial, viral, and other pathogenic threats that can infiltrate the joint and cause an infection and internal joint damage, which may lead to secondary OA.
- An occupation that requires you to overuse certain joints
- Cigarette smoking (4)
- Gender: Women are more prone to OA than men (5)
- Increasing age
- Nerve injury
- Underlying joint abnormality (6)
- Weak thigh muscles
- Bone deformities
- Diabetes
Complications
In some cases, the OA-induced joint damage can become severe enough to cause the following complications:
- Chondrolysis, a condition marked by the rapid and total destruction of the cartilage in the joint
- Osteonecrosis, which refers to bone death
- Hairline fractures, usually in the wake of repeated injury or stress
- Joint infection
- Internal bleeding within the joint
- Breakdown or rupturing of the supportive tendons and ligaments that hold the joint in place, which leads to joint instability
- Pinched nerve, especially in the case of OA of the spine
When to See a Doctor
OA needs medical evaluation and treatment, so it is important that you see a doctor as soon as you notice the first symptoms.
Look out for the following warning signs as they might indicate OA:
- One or more joints become painful, swollen, warm to the touch, or unusually red and stiff.
- The joint symptoms do not subside within 3 days or more.
- Multiple flare-ups of joint symptoms occur within a month.
The doctor will conduct the necessary examination to reach a conclusive diagnosis and then design a treatment plan that will be customized to your individual case.
Final Word
OA tends to worsen with age and can progress to cause joint deformity and even disability if not met with proper care and treatment. Also, the constant pain and stiffness in the joints can keep you from performing the simplest of tasks and hamper your overall quality of life.
Since there is no permanent cure for OA, the best you can do is manage it properly through a multidimensional treatment approach that is customized to your individual needs.
Your doctor will take into account your age, severity of your symptoms, and other relevant health factors to recommend the appropriate medication, exercises, supportive devices, diet, lifestyle tips, and other useful interventions to reduce the frequency and intensity of flare-ups.

- Was this article helpful?
- YES, THANKS!NOT REALLY


