In this article:
Osteoarthritis (OA) is the most common type of joint disease in the United States, affecting over 30 million people. (1) Approximately 37% of people over the age of 60 have radiographic evidence of OA of the knee, and up to 19% have symptomatic knee arthritis. (2)

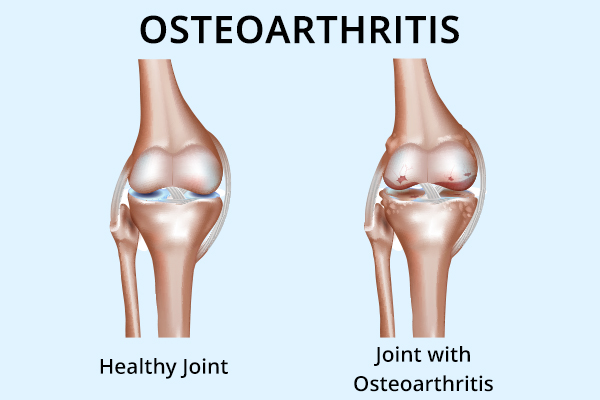
OA is a degenerative disorder characterized by the progressive thinning and breakdown of cartilage that causes damage to the underlying bones, leading to pain, swelling, and deformity.
Although this kind of tissue degeneration can occur in any joint, it is more common in:
- Weight-bearing joints, such as the knees, lower back, hips, and feet
- Overused joints, such as the neck, hands, and fingers
OA can affect people of all ages and gender.
Treatment for Osteoarthritis
While OA can’t be cured, various treatments are available to help reduce the pain and swelling. Moreover, emerging regenerative medicine treatments hope to slow the disease progression.
It is crucial to obtain a correct diagnosis and treatment plan with your physician.
- In some instances, injections of medication directly into the affected joint may be helpful. This is usually performed by a rheumatologist or orthopedist.
- For advanced knee and hip OA, joint replacement surgery is often quite successful.
Diagnosing Osteoarthritis
A physical examination by an experienced physician, such as a rheumatologist or orthopedist, is the best way to diagnose OA. An X-ray is helpful and can reveal cartilage loss, deformities, and calcifications and can confirm the physical exam findings.
Dietary Recommendations for Osteoarthritis
Diet and nutrition have a significant impact on arthritis, and numerous published studies have demonstrated improvements in arthritis symptoms with dietary modifications. (3)(4)
1. Avoid foods that can contribute to inflammation (pro-inflammatory)
Some foods increase inflammation in the body and worsen the pain, swelling, and stiffness associated with arthritis.
- While there is no single dietary approach that works for all, it is best to avoid added sugars, refined carbohydrates, and fried and processed foods. This also helps prevent calorie excess, thus aiding in managing your body weight to limit the excess load on the joints.
- You may also be advised to limit gluten, dairy, red meat, corn, and sometimes even eggs and soy-based products.
The only way for patients with arthritis to determine if any of these foods should be avoided or not is by simply trying their own elimination diet and observing how they respond.
2. Consume foods that help reduce inflammation (anti-inflammatory)
Some foods contain anti-inflammatory properties that help subside the swelling and pain in the body.
The Mediterranean diet has been demonstrated in studies to improve arthritis symptoms. (5) This “anti-inflammatory” diet emphasizes the intake of fish, monounsaturated oils such as extra virgin olive oil, and whole foods that include leafy green vegetables, fresh fruits, whole grains, and legumes.
3. Take help of supplements if required

You must take vitamin and nutritional supplements only upon your doctor’s recommendation.
- Glucosamine and chondroitin sulfate are the most commonly used nutraceutical and help about 50% of OA sufferers. (6) They are quite safe and free of drug interactions. They contain building blocks for cartilage tissue and thus may reduce joint degeneration.
- Fish oil and related omega-3 fatty acids have been shown to reduce joint inflammation and have been found useful in some studies. (7)(8)
- Curcumin, a turmeric extract, is a popular product and a well-researched natural anti-inflammatory agent. (9)(10)
- Undenatured collagen has also demonstrated benefits in clinical trials. (11)
- Other supplements that have shown some benefit in clinical studies include pycnogenol (maritime pine bark extract), avocado/soybean extracts (unsaponifiable), Boswellia (Indian frankincense), MSM and, SAMe. (12)(13)(14)(15)(16)
- Wobenzym, a mixture of enzymes developed in Germany, was found to be an effective natural anti-inflammatory nutraceutical. (17)
Exercise for Osteoarthritis

Maintaining range of motion in the joint, flexibility of the associated ligaments, and strong musculature is very important and an essential part of a complete treatment program for OA.
- High-impact exercises should be avoided, but walking, swimming, yoga, and limited resistance exercise are recommended.
- Physical therapy is often quite beneficial.
- Protect the joints from injury with low-impact exercises and the use of protective gear when necessary.
- Experienced personal trainers can help develop specific exercise programs to enhance joint function.
Difference Between Rheumatoid Arthritis, Arthritis, and Osteoarthritis
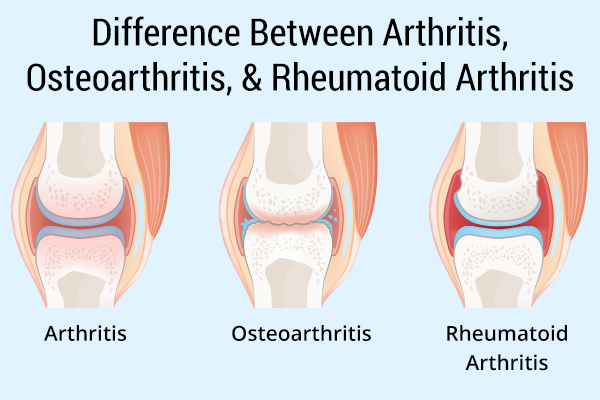
Rheumatoid arthritis (RA) is a systemic autoimmune condition in which the immune system attacks the tissues within the joints, resulting in joint damage.
Less common than OA, it occurs in about 1% of the population and afflicts people at any age, even children. RA commonly affects multiple joints simultaneously.
OA is typically seen in older people and is mostly an aging phenomenon in which degeneration and cartilage damage of the joints take place, usually impacting a limited number of weight-bearing joints.
“Arthritis” is a broad term that refers to joint inflammation. There are many different types of arthritis, of which OA is the most common.
Osteoarthritis Flare-Ups During Cold and Damp Months
The joint tissues are sensitive to changes in barometric pressure, which can cause swelling and stiffness. This is why many people with arthritis can predict rain before the weatherman.
In colder environments, connective tissues that surround the joints, such as the ligaments and muscles, harden and lose flexibility. These actions irritate the joints and make them stiff. Low temperatures also reduce blood flow to the joints, aggravating OA.
Risk Factors for Osteoarthritis
The exact causes of OA are poorly understood, but the risk factors are well known: (18)
- Age: The incidence of OA rises along with age.
- Gender: Women are affected more often than men.
- Genetics: Over 50% of the risk of OA is due to genetic factors. (19)
- Obesity: Excess load on the joints increases the wear and tear and stresses the joints, especially the knees, hips, and spine. Persons with a BMI of >30 have seven times the risk of developing OA of the knees. (20)
- Trauma and injury: Previous events such as motor vehicle accidents or sports injuries increase the risk of OA in later years.
- Occupation: Certain repetitive activities required for workers in construction, firefighting, forestry, and agriculture increase the risk of OA, especially of the knees and spine.
- Inactivity: A sedentary lifestyle actually increases OA risk. Physical activity is generally protective of the joints, although some runners will experience OA of the knee and hip.
Complications Associated With Osteoarthritis

OA can cause the following problems in the long run, especially when left untreated:
1. Fatigue
The simple act of rising from a chair and climbing a flight of stairs can be painful and requires exaggerated effort by a person living with arthritis.
When everyday activities become painful and require extra effort, fatigue tends to set in. (21)
2. Joint deformity
The advancing joint deformity and pain associated with untreated OA can lead to disability, chronic pain, and the inability to walk and participate in desired activities.
3. Joint damage
In some cases, OA may lead to severe joint damage that requires surgery, such as replacement of the knee or hip joint.
Final Word
While there is no specific treatment for osteoarthritis, dietary modifications may help improve the symptoms. However, there is no single dietary approach suitable to all.
It is vital to consult a doctor and follow the recommended treatment plan to slow down the progression of the disease and manage symptoms.
- Was this article helpful?
- YES, THANKS!NOT REALLY


